Table of Contents
Cognitive Behavioural Therapy for Insomnia (CBT-I)
Primer
Cognitive Behavioural Therapy for Insomnia (CBT) is a structured, time-limited psychotherapy that treats insomnia disorder. It is an effective and cost-effective treatment for insomnia disorder and should be offered as a first-line treatment.[1][2] Research evidence has also shown that CBT-I should also be a first-line treatment for insomnia in mid-life women experiencing menopause with hot flashes.[3] With the advent of the internet, CBT-I has become widely accessible online (see table below), and is of similar efficacy with in-person CBT-I.
Indications
- Insomnia disorder
- Major depressive disorder with comorbid insomnia
- Research evidence has also shown that CBT-I should be a first-line treatment for insomnia in mid-life women experiencing menopause with hot flashes.[4] With the advent of the internet, CBT-I has become widely accessible online (see table below).
Efficacy
- Patients generally see improvements in sleep within the 2 to 3 weeks of starting CBT-I.
- There is strong and robust evidence that shows the effectiveness of CBT-I for insomnia.[5]
- Importantly, there is comparable treatment effect with hypnotics, and the effects from CBT-I are more durable than medications.[6]
- CBT-I can also reduce and eliminate the need for hypnotic use and significantly reduce depression symptoms.[7]
Length
- The typical duration of a course of CBT-I lasts for about 6 to 12 sessions.
Advantages
CBT-I is more advantageous than medications for 3 key reasons:
- CBT-I is equally as effective (or more effective) as any medication used for insomnia
- There are no side effects from CBT-I (unlike medications)
- The gains from CBT-I are durable and sustaining (unlike medications)
Delivery
CBT-I can be delivered in various formats with similar success rates, including through:
- One-on-one in person therapy
- Online CBT-I (via websites)
- Bibliotherapy (self-guided CBT-I books)
The 3P Model
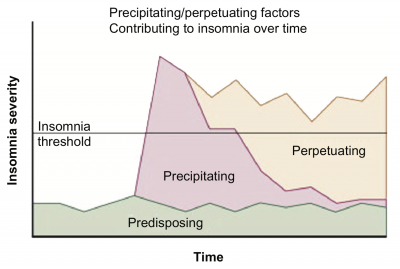
The three “Ps” (3P) model of insomnia describes how predisposing, precipitating, and perpetuating factors can lead to the development of insomnia:
- Predisposing Factors
- Circadian preference (body clock)
- Sleep temperament
- Early trauma and adversity
- Precipitating Factors
- Acute stressors (e.g. - job loss, caring for newborn)
- Mental disorders (e.g. - depression)
- Perpetuating Factors
- Physical and mental tension
- Sleep defeating worries
- High sleep effort
- Compensatory efforts
- Napping
- Resting
The use of cognitive and behavioural strategies in CBT can help modify these above factors.
Education
Providing the patient education that the beginning of CBT-I helps frame the structure of the therapy. This includes providing education about the role of sleep and the body clock, and the basic principles of CBT-I.
The Body Clock
- The body clock is a 24 hour clock, and influences the timing of behaviours of sleep, physiological processes
- Melatonin is a hormone released by the brain that is a:
- Time-setter and mild sedative
- Melatonin level rises 3-5 hours before sleep onset (0.1 to 0.5mg is enough to do this)
- Melatonin levels are typically lower during the day
- Melatonin is also suppressed by blue light (computer screens)
- Bright morning light is the most powerful time setter and keeps the body clock on a regular schedule
- The natural sleep window is between 12am to 9am
- Body has a high level of alertness towards the end of the day
- Sleeping outside this window is depressogenic and increases the risk for “social jet lag.”
- Napping is like having a snack before dinner (takes away your appetite)
- Prior to bed, you want to do low arousal activites
- Unhelpful beliefs about sleep can affect our sleep
- “I need 8 hours to sleep to function tomorrow”
- “I can’t sleep without medications”
- Conditioned Arousal
- If you’re used to doing things in bed, like watching TV, or playing on the phone, you can also condition yourself to not sleep in bed.
What is CBT-I?
- The goal of CBT-I is to join your fragmented sleep together
- Waking up late on the weekends = artificial jet lag (e.g. - waking up 3 hours difference between weekday and weekend is like a 3 time zone jet lag!)
- Staying up late is easier than falling asleep earlier, and CBT-I helps “retrain” this
- Physician and patient should work together to find a good wake time that works for the patient
- If sleepy but starting to nod off and doze, stand up, walk, do anything but lie down!
- 2 hours before bedtime no bright lights or phones (to avoid inhibiting your melatonin production)
- Telling a patient to just “relax their minds” at night doesn’t work – they'll end up thinking of everything
- If there are middle of the night awakenings:
- Go to another room: best to do something very repetitive and boring (e.g.- word searches); crossword puzzles and Sudoku are in fact highly stimulating (since people are searching and thinking of answers or doing math)
- Also don’t read magazines or books, or you might be motivated to finish it!
- Once you get head-nodding feeling, then go back to sleep!
- Always cover the clock at bedtime, to avoid the mental math of “How many hours do i have until I wake up?”
Principles
The principles of CBT-I is to correct unhelpful sleep-related beliefs and anxiety as well as common sleep-disruptive habits that maintain or contribute to insomnia. Patients are advised to adhere to basic rules regarding their sleep, including:
- Rule 1: Select a standard wake-up time everyday (including the weekends!)
- Rule 2: Use the bed only for sleeping (or sexual activities)
- Rule 3: Get up when you can’t sleep
- Rule 4: Don’t worry, plan, etc., in bed
- Rule 5: Avoid daytime napping
- Rule 6: Only go to bed when you are sleepy, but not before the time suggested by your doctor
Components
Treatment during CBT-I involves all or some of the following components:
- Sleep restriction therapy
- Reduce the time in bed, to match the amount of sleep you produce
- Stimulus control
- Do low arousal activities to stimulate sleepiness
- Sleep hygiene (on its own not very effective)
- Relaxation training (e.g. - progressive muscle relaxation)
- Cognitive strategies
Sleep Restriction
Sleep restriction involves:
- Tracking your sleep for 2 weeks using a sleep diary to determine the average nightly total pre-existing sleep time
- Then calculate a sleep window or “total time allowed in bed.” This is the average nightly total pre-existing sleep time + 50% of the time that the patient is awake in bed (e.g., if it takes 1 hour to fall asleep, and the patient is up for another 1 hour mid-sleep, and they only sleep for 6 hours, then their sleep window is 7 hours in bed).
- On follow-up, the sleep window is lengthened or reduced based on the calculated sleep efficiency (SE).
- The patient is told to increase or reduce their time in bed by 15-30 minutes (i.e., pushing bedtime later or earlier) until the SE reaches around 85%. The wake time is kept the same every week.
- Stimulus control principles are reinforced throughout.
Stimulus Control
Stimulus control is one main technique of CBT-I. The goal of stimulus control is to train the mind to associate the bed and bedroom with being asleep. This includes making it a point to get out of bed if one has not fallen asleep after a certain amount of time (e.g. - 20 minutes). The more often one does other things in bed (e.g. - watching TV, reading, lying down without sleeping, ruminating/being anxious) the weaker the association gets between bed and sleeping. The goal is to re-establish a strong association between being in bed and sleeping.
Stimulus control involves:
- Adhering to stimulus control principles (see list)
- Reversing the conditioning process of associating the bedroom and bedtime with insomnia.
- Reestablishes regular circadian rhythm by association of appropriate time and environment with sleep onset.
Stimulus Control Principles
- Go to bed only when sleepy. This time may be different each night, and that is okay.
- Wake up every day at the same time regardless of how tired you are.
- If you wake up in the middle of the night, get out of bed, go to another room, and return when sleepy again.
- Use the bed only for sleep or sexual activity.
Relaxation Therapy
Relaxation therapy involves reducing the somatic and/or mental ruminations that interferes with sleep and include techniques such as:
- Progressive muscle relaxation
- Imagery training
- Autogenic training
- Meditation
Cognitive Therapy
Cognitive therapy involves correcting faulty expectations, cognitive distortions, and false beliefs that interfere with sleep by:
- Avoiding blaming insomnia for all daytime impairments or difficulties
- Encouraging the patient to keep realistic expectations of sleep requirements and daytime alertness (“It is okay if you only get 3-4 hours of sleep on one night during the course of CBT-I.”)
- Avoiding catastrophizing after a poor night’s sleep (“Insomnia is unpleasant but not life threatening.”)
- Exploring cognitive experiments:
- If rumination and anxiety affects sleep initiation, set aside “worry time” earlier in the evening before bed.
- Trying to keep oneself awake as long as possible (also known as paradoxical intention).
Sleep Hygiene
Sleep hygiene involves correction of lifestyle and environmental factors that interfere with sleep. While good sleep hygiene is important for any healthy sleep, chronic insomnia rarely is due to only poor sleep hygiene alone.
- Keep Your Bedroom Cool, and Dark: A dark room reminds your brain it is nighttime, and a cool room temperature allows your body thermoregulate during sleep.
- Get Regular Sleep: Make sure your sleep schedule is regular. Wake up the same time every day and go to sleep the same time every day. This includes the weekdays and weekends.[8]
- No Napping: Do not nap at all during the day. This includes lying down! It is important to associate a horizontal body position with sleeping.
- No Stimulants: No caffeine or smoking (at least 8 hours before bed)[9]
- No Electronics Before Bed: Do not watch televisions, use your phone, or a computer for at least 1 hour before bed. The blue light stimulates the brain to think it's daytime again.
- Have A Bedtime Routine: Set a bedtime routine before going to bed (i.e. - 30 minutes before sleeping, turn off all electronics, listen to soothing music, and read a book in a dim light)
- Wind Down: Make sure you are winding down at least 1 hour before bed, and avoid doing stimulating activities
- Only Sleep When You Are Sleepy: Do not go to bed until you are actually feeling sleepy
- Don't Lie Down During the Day: You want to associate a horizontal body position only with sleeping.
- Environment: Make sure the room is quiet, not too bright, and at the right temperature (not too warm or cold)
- Bed For Sex and Sleep Only: Do not read books, use your phone, or use a computer on the bed. It is important to associate the bed with sleep (and sex if applicable…) and not any other activities.
- Don't Look At The Clock: Avoid the temptation to peek at the clock!
- Don't Use The Snooze Button: Snoozing results in short-term gain with long-term (bad) consequences. Snoozing can worsen sleep the day after.
- Keep a Sleep Diary: A sleep diary can help make sure you know exactly when you sleep and wake up, and help direct the right changes.
Resources
Online
Online Insomnia Therapies
| Name | Description | Cost |
|---|---|---|
| Slumber Camp | Excellent simple to use, weekly guided CBT-I course | $29 USD |
| Free CBT-I | Website providing general CBT-I sleep tips in multiple languages | Free |
| CBT for Insomnia | 5-session on-line cognitive behavioural therapy (CBT) program for insomnia. | $24.95 US to $49.95 US |
| CBT-i Coach | Structured program that teaches strategies to improve sleep and help alleviate symptoms of insomnia. | Free |
| Sleepio | Evidence-based CBT-I online and mobile app program | $300 US for a 12-month subscription |
| SlumberPRO | Self-help program from Queensland Australia, requires 30-60 minutes each day and program lasts 4-8 weeks | $39 AUS |
| Go! To Sleep | 6-week CBT-I program (and mobile app) available through Cleveland Clinic of Wellness | $3.99 US for app, or $40 US for web |
| SHUTi | 6-week CBT-I program, evaluated in 2 randomized trials involving adults with insomnia and cancer survivors | $135 US for 16 weeks access, or $156 US for 20 weeks access |
| Restore CBT-I | A 6-week CBT-I program evaluated in a randomized trial | £99 to £199 |
| Sleep Training System | 6-week on-line CBT-I program with money-back guarantee and personalized feedback | $29.95 US |