- Last edited on January 4, 2024
Cognitive Behavioural Therapy (CBT)
Primer
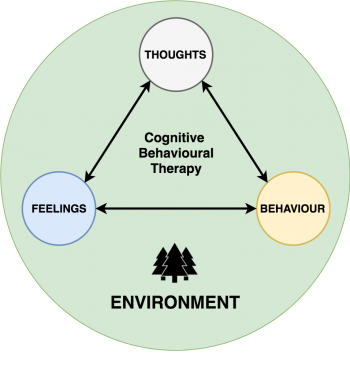
Cognitive Behavioural Therapy (CBT) is a structured, time-limited (usually 12-16 sessions) psychotherapy that identifies and addresses persistent maladaptive thought patterns to change emotions (e.g. - depression/anxiety/trauma) and behaviours (low motivation/insomnia). It uses strategies such as goal-setting, breathing techniques, visualization, and mindfulness to decrease emotional distress and self-defeating behaviour. Treatment is generally time-limited. CBT can be delivered in a wide variety of formats, including in groups and via remote delivery (online or phone). Although most commonly used for depression and anxiety, CBT has also been specialized to treat other conditions, such as CBT for insomnia (CBT-I) for insomnia disorder, and trauma-focused CBT (TF-CBT) for post-traumatic stress disorder.
Indications
- CBT is used as monotherapy or in combination with medication for major depressive disorder, generalized anxiety disorder, panic disorder, posttraumatic stress disorder, social phobia, somatic disorders, chronic pain, insomnia, and eating disorders.
- CBT with exposure response prevention (ERP) is used on the treatment of obsessive-compulsive disorder.
- If a patient has cognitive distortions and avoidance behaviour, this make them a good candidate for CBT.
How Does It Work?
CBT techniques include identifying distortions such as overgeneralization of negative events, catastrophizing, minimizing positive events, and maximizing negative events. Patients work with therapists to identify and change cognitive distortions and avoidance behaviours that cause their symptoms. This frequently involves keeping diaries or “thought records” outside of sessions and practicing behavioural strategies learned in sessions.
- CBT is based on an ever-evolving formulation of patients’ problems and an individual conceptualization of each patient in cognitive terms.
- CBT requires a good therapeutic alliance (true for all psychotherapies).
- CBT focuses on collaboration and active participation. Both the therapist and patient should view therapy as teamwork. Together they decide what to work on for each session, how often to meet, and what to do between sessions for therapy homework. At first, the therapist may be more active in suggesting a direction for therapy sessions and in summarizing what's discussed during a session.
- CBT is goal oriented and problem focused. You should ask in your first session for your patient to describe their problems and set specific goals so there is a shared understanding of what they are working towards.
- Self-perception is amenable to change through CBT
Components of CBT
The key components of CBT include:
- Psychoeducation about anxiety and feared situations
- Goal setting, self awareness (thoughts-feelings-behaviours)
- Cognitive restructuring to address maladaptive thinking and learning coping skills and focused thinking
- Somatic management techniques (relaxation training)
- Deep breathing
- Progressive muscle relaxation (PMR)
- Guided imagery
- Gradual, systematic exposure to feared situations
- In vivo (in the real situation)
- Imaginal (imagining the situation)
- Live modeling (demonstration of non fearful response)
- Behavioural activation
- Increasing engagement in adaptive activities (things that increase pleasure or mastery)
- Decrease engagement in activities that maintain or increase the risk for the symptoms
- Relapse prevention
- Booster sessions of CBT
Efficacy
Length
- The average length of a course of CBT lasts between 12 to 16 sessions (i.e. - weeks), with each session of about 50 minutes in length. The course of CBT may be longer or shorter depending on the disorder and severity of symptoms.
Terminology
CBT uses lots of different terminologies, and it can be helpful to spell out exactly what they mean, so both you and your patients can be speaking the same language.
Definitions in CBT
| Description | What to Tell Your Patient | |
|---|---|---|
| Feelings | • Feelings are one word (e.g. - “happy, sad, excited”) | “A person can't change their feelings, but they can change their thoughts and behaviours.” |
| Thoughts | • Thoughts are sentences that run through one's mind. One can have many different thoughts about a situation. | • “Sometimes thoughts are right, but sometimes they can be wrong too” • Thus, be skeptical of your thoughts! |
| Actions/Behaviours | • Actions and behaviours are the things one does, and one's behaviours. Thoughts influence actions and behaviours. | - |
Core Beliefs
Core beliefs are fundamental assumptions (not truths) that individuals have made about about themselves, others, and the world. These beliefs develop over the course of their lives. Core beliefs influence how a person sees the world around them and themselves. Core beliefs are usually so connected to a person's identity that they stop noticing them or questioning these beliefs. For example, someone in a depressive episode might think “I am a failure” and because these beliefs are not questioned and assumed to be “100% true,” the individual lives and acts as though they beliefs are real and true.
Beck's Cognitive Triad
Beck's cognitive triad, also known as the negative triad, is a cognitive-therapeutic model of the three key elements of a person's belief system when going through depression. The triad involves automatic, spontaneous and seemingly uncontrollable negative thoughts about:
- The self – “I'm worthless and ugly” or “I wish I was different”
- The world – “No one values me” or “people ignore me all the time”
- The future – “I'm hopeless because things will never change” or “things can only get worse!”
Automatic Thoughts and Cognitive Distortions
Thoughts can often come automatically, and CBT challenges us to think more closely about these thoughts. Some automatic thoughts are true, but many are either untrue or have just a grain of truth. CBT requires patients to use a structured method to evaluate their thinking. Otherwise, their responses to automatic thoughts can be superficial and unconvincing and will fail to improve their mood or functioning. Typical automatic thoughts (also called cognitive distortions) include:
Common Automatic Thoughts or Cognitive Distortions
| Cognitive Distortion | Definition | Automatic Thought |
|---|---|---|
| All-or-nothing thinking | Viewing a situation in only two categories instead of on a continuum. | “If I’m not a total success, I’m a failure.” |
| Catastrophizing | Predicting the future negatively without considering other, more likely outcomes. | “I’ll be so upset, I won’t be able to function at all.” |
| Emotional reasoning | Thinking something must be true because you “feel” (actually believe) it so strongly, ignoring or discounting evidence to the contrary. | “I know I do a lot of things okay at work, but I still feel like I’m a failure.” |
| Disqualifying or discounting the positive | Unreasonably telling yourself that positive experiences, deeds, or qualities do not count | “I did that project well, but that doesn’t mean I’m competent; I just got lucky.” |
| Labeling | You put a fixed, global label on yourself or others without considering that the evidence might more reasonably lead to a less disastrous conclusion. | “I’m a loser. He’s no good.” |
| Magnification/minimization | When you evaluate yourself, another person, or a situation, you unreasonably magnify the negative and/or minimize the positive. | “Getting a mediocre evaluation proves how inadequate I am. Getting high marks doesn’t mean I’m smart.” |
| Mental filter (Selective abstraction) | When you have a tendency to focus on only one detail (often taken out of context) and ignore all other aspects and more important parts of a situation (e.g. - “seeing the glass as half empty”). | “Because I got one low rating on my evaluation [which also contained several high ratings] it means I’m doing a lousy job.” |
| Mind reading | You believe you know what others are thinking, failing to consider other, more likely possibilities. | “He thinks that I don’t know the first thing about this project.” |
| Overgeneralization | You make a sweeping negative conclusion that goes far beyond the current situation. | “[Because I felt uncomfortable at the meeting] I don’t have what it takes to make friends.” |
| Personalization | You believe others are behaving negatively because of you, without considering more plausible explanations for their behavior. | “The repairman was curt to me because I did something wrong.” |
| “Should” and “must” statements | You have a precise, fixed idea of how you or others should behave, and you overestimate how bad it is that these expectations are not met. | “It’s terrible that I made a mistake. I should always do my best.” |
| Tunnel vision | You only see the negative aspects of a situation. | “My son’s teacher can’t do anything right. He’s critical and insensitive and lousy at teaching.” |
| Magical thinking | Believing that the course of events in the world depends on your actions and thoughts. | “I need to wash my hands 10 times each time, or else my parents will die.” |
Emotional Reasoning Example
Try this out!- Write this down on sheet of paper: “I will win the lottery on Friday, Jan 22”
- Then write this down on sheet of paper: “My mother will win the lottery on Friday”
- Finally, write this down on sheet of paper: “My mother will die on Friday Jan 20th”
Notice how the first two sentences don't provoke many emotions, but the third sentence is “emotional reasoning,” you might be “reading” into this feeling, thinking: “Might I be jinxing the universe by writing this down?!” This is a tough thing to overcome for individuals who struggled with the cognitive distortion of emotional reasoning every day.
Structure
Intake Assessment
- Identify your patient's current feelings (“I’m a failure, I can’t do anything right, I’ll never be happy”)
- Identify the problematic behaviours (isolating herself, spending a great deal of unproductive time in her room, avoiding asking for help). These problematic behaviours both flow from and in turn reinforce Sally’s dysfunctional thinking.
- What the precipitating factors that in influenced your patient's perceptions at the onset of their depression? (e.g., being away from home for the first time and struggling in her studies contributed to her belief that she was incompetent)
- Third, I hypothesize about key developmental events and how the enduring patterns of interpreting these events that may have predisposed your to their symptoms (e.g., your patient has had a lifelong tendency to attribute personal strengths and achievement to luck, but views her weaknesses as a reflection of her “true” self).
Goal Setting
It is important for the patient to have specific goals they want to achieve by the time they are finished the course of therapy. It is also important to have goals between sessions, that are more attainable and realistic. The SMART goals framework is one way of achieving that. A goal should feel 80% do-able and 20% challenging so as to strike the right balance.
S- Specific (well defined, clear, and unambiguous)M- Measurable (specific way to measure your progress towards the goal)A- Attainable (something not impossible - “Do something 80% attainable and 20% hard”)R- RealisticT- Time (must have a start and finish date - if the goal is not time constrained, there will be no sense of urgency to achieve the goal!)
Example of a SMART goal could be: “Add more structure to your day” (i.e. - make your bed, eat regular meals, have a regular sleep schedule, and make a regular schedule). Another SMART goal could be: “Have more social interaction by calling one friend each week.”
First Session
- Outline that there are tasks (“homework”) for each week, and doing the task is like taking medication. Homework is a vital part of therapy and it is important that the patient is aware of this in the first session.
- Buy a guide book, such as Mind Over Mood
- Outline that there are about 16 sessions in total, again, like medication, it is important to do this
- Get a journal to keep a thought record, and begin doing thought records early
- Photocopy the homework if possible
- Do scales for whatever disorder you're addressing:
- PHQ-9 or Beck Depression Inventory for Depression
- SPIN for Social Anxiety
- The way you think, affects how you feel and how you behave
- Identify specific problems, and set specific goals
- E.g. - problem = isolation, goal (is something behavioural) = start new friendships, and spend more time with existing friends
- During future sessions, and in discussing how to improve day-to-day routines, you will help your patient evaluate and respond to thoughts that interfere with the goals described above, such as: My friends won’t want to hang out with me,“ or “I’m too tired to go out with them.”
- You will help the patient evaluate the validity of her thoughts through an examination of the evidence. They should be able to test the thoughts more directly through behavioural experiments, where they initiate plans with friends. Once your patient recognizes and corrects the distortion in their thinking, they will benefit from more straightforward problem solving to decrease their isolation.
Homework to Assign after Session 1
- Define a goals list
- Begin a thought record. Remind yourself to be skeptical of these thoughts and that they may not always be true
- Be kind to yourself
- Think about things you want to bring up at the next session
- Organize an activity to do (this is “behavioural activation”)
Agenda Setting
Just like how CBT is a structured-form of therapy, your sessions with your patient should also be structured and modeled on that. A typical CBT session should be structured as follows:[7]
CBT agenda based on a 60 minute session
| Time | Focus | Description |
|---|---|---|
| Before appointment | Assess symptoms | Patient fills out a scale assessing symptoms (GAD-7, PHQ-9, Beck) |
| 5-10 minutes | Check-in | What happened last week? Do a “mood check”: how is this week's mood compared to last week's? |
| 5 minutes | Set the Agenda | Decide: what are the important things that happened that need to be problem-solved today? Prioritize the agenda if there are many problems that happened. |
| 5 minutes | Bridge | Connect back to the last session: what was important during the last therapy session? |
| 5 minutes | Homework | Review homework done over the past week. |
| 30 minutes | Problem Solving | Focus on the core themes of CBT and problem-solve. |
| 5 minutes | Wrap up | Ask patient for feedback: How did the session go? Is there anything that bothered them or that they didn’t understand? Is there anything they'd like to see changed in future sessions? Assign homework for the next session |
Homework
Homework is an integral part of CBT, and what makes CBT work. There are various types of homework assignments including:
- Behavioural activation
- Monitoring automatic thoughts
- Practicing new skills or implementing new solutions
- Reading assignments (like chapters in Mind Mover Mood)
When Homework Isn't Done
You should ask yourself what is going through your mind when homework isn't being done. Remind yourself that you are not doing your patients any favours if you allow them to skip homework or don't encourage better compliance. The literature shows that patients who do homework assignments regularly have a better prognosis that paints who do not.[8]Thought Records
Thought records are done outside of the CBT session, where patients record their automatic thoughts and feelings over the week:
- Rating their feelings
- Noticing which thought matches the feeling
- Rating how much you believe in each thought
- Rating which thought is the most therapeutic
- Evidence for and against the thought
Vague Thought Records
It can sometimes be hard to describe what exact situation occurred when your patient describes their automatic thought to you weeks after the event. By that time, the patient often has had several days to think about their actions-thoughts-behaviours, and it can be easily to over-rationalize those thoughts. To get a better sense of the exact automatic thought and behaviours, it can be helpful to ask your patient: “replay everything back to me like a movie, down to the specific words exchanged and the conversation if you can.” This helps ground the patient on the exact situation at that time, and helps you better understand their thought process.Balancing Thoughts
The goal of CBT is to help your patients correct the automatic thought (sometimes called “hot thought”), by reaching balanced thoughts (e.g. - “Even though [I’m behind on my rent], I can see that [I have a solution now/and a capable person], because [I have support from my family].”) Beware though, of superficial and “fake” balance thoughts. For example, if a patient is constantly worried about having anxiety because their thought is: “I’m a terrible mom.” and her balanced thought is “but I’m a good wife.” Notice that this balanced thought doesn't actually relate to the thought. If the balancing thought does not correspond with the automatic thought, that’s a pitfall the therapist must identify!
Questioning Automatic Thoughts
When addressing automatic thoughts or cognitive distortions, the following questions can be helpful:
- What is the evidence that supports this idea? What is the evidence against this idea?
- Is there an alternative explanation or viewpoint?
- What is the worst that could happen (if I’m not already thinking the worst)? If it happened, how could I cope? (What is the best that could happen? What is the most realistic outcome?)
- What is the effect of my believing the automatic thought? What could be the effect of changing my thinking?
- What would I tell [a specific friend or family member] if he or she were in the same situation?
- What should I do?
Tips and Techniques
When evaluating situations that your patient brings up, here are some helpful techniques:
Piecharts
- Use a pie chart to assess the pie chart contribution of the situation
Percentage Scales
- “If you are a terrible student, then where are you on this continuum,” “Are you a 100% terrible student? 50%? or 0%? Why that percent?”
- “If you feel like you are a failure or people don’t love you, “How much of that do you think is true? 100%, 50%?”
Socratic Questioning
Socratic questioning, or the socratic method, is a key technique in CBT. You help your patient understand themselves by asking questions about their thoughts, examples include:
- “What was going through your mind before you started to feel this way?”
- “What images or memories do you have of this situation?”
- “What does this thought mean about your future, and your life?”
- “What are you afraid might happen?”
- “What is the worst that could happen?”
- “What does this mean about how the other person thinks about you?”
- “What does this mean about the other person or people in general?”
- “Did you break rules, hurt others, or do something that you should not have done?”
- “What do you think about yourself about having done this, or thinking you did this?”
Therapeutic Alliance
- Note any changes in therapeutic alliance, transference/countertransference
When emotions are too much
- When a patient's feelings and thoughts are very valid, and the patient is unable to see alternative ways of scrutinizing them, another one way to help a patient reframe their situation is to ask them how well do they cope with these feelings?
Resources
For Patients
- Mind Over Mood - Teaches skills and principles used in cognitive behavioral therapy, provides worksheets, assignments
- MoodGym - Interactive self-help program for preventing and coping with depression and anxiety; teaches self-help skills drawn from CBT