- Last edited on February 26, 2023
Approach to Stroke
Primer
A stroke (also called a cerebrovascular accident, CVA) is an acute disturbance of the cerebral perfusion or vasculature. Approximately 85% of strokes are ischemic (blockage of a vessel) and remainder are hemorrhagic.
Risk Factors
CHA₂DS₂-VASc Score
Ntaios G, et al. CHADS2, CHA2DS2-VASc, and long-term stroke outcome in patients without atrial fibrillation. March 12, 2013 80:1009-1017| Criteria | Points |
|---|---|
| Age | • <65 years old = 0 • 65-74 years old = +1 • ≥75 years old = +2 |
| Sex | • Male = 0 • Female = +1 |
| Congestive heart failure history | +1 |
| Hypertension history | +1 |
| Stroke/TIA/thromboembolism history | +2 |
| Vascular disease history (Prior MI, peripheral artery disease, or aortic plaque) | +1 |
| Diabetes mellitus history | +1 |
CHA₂DS₂-VASc Score Interpretation
Lip G et al. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010 Feb;137(2):263-72. doi: 10.1378/chest.09-1584. Epub 2009 Sep 17.| CHA₂DS₂-VASc Score | Risk of ischemic stroke | Risk of stroke/TIA/systemic embolism |
|---|---|---|
| 0 | 0.2% | 0.3% |
| 1 | 0.6% | 0.9% |
| 2 | 2.2% | 2.9% |
| 3 | 3.2% | 4.6% |
| 4 | 4.8% | 6.7% |
| 5 | 7.2% | 10.0% |
| 6 | 9.7% | 13.6% |
| 7 | 11.2% | 15.7% |
| 8 | 10.8% | 15.2% |
| 9 | 12.2% | 17.4% |
Etiology
Strokes can be caused by anyone of the following pathophysiological processes:
- Large artery atherosclerosis (20%)
- Small vessel lacunar (lacunar = deep vessels) stroke (25%)
- Cardioembolism (due to arrythmias such as atrial fibrillation) (20%)
- Cryptogenic (i.e. - cannot be determined) (30%)
Atherosclerosis, Atrial Fibrillation (Cardioembolism), and Stroke Risk
- Anytime an individual has atrial fibrillation, there is an increased stroke risk!
- If an individual symptomatic carotid stenosis, with symptoms such unilateral weakness or amaurosis fugax (i.e. - transient loss of vision in one eye), there is a 25% chance of stroke in the next year!
- Therefore, for these individuals it is recommended that the receive a carotid endartectomy
- If asymptomatic, they be can treated with anti-platelets
Stroke Presentations
Anterior Cerebral Artery (ACA)
- Location: cerebral hemisphere, medial aspect
- Typical presentation: more motor symptoms
- Symptoms:
- Leg weakness > Arm weakness
- Abulia (diminished motivation)
- Paralysis of foot and leg with or without paresis of arm
- Cortical sensory loss over leg
- Grasp and sucking reflexes
- Urinary incontinence
Middle Cerebral Artery (MCA)
- Location: cerebral hemisphere, lateral aspect
- Typical presentation: affects speech and eye movements
- Symptoms:
- Hemiparesis
- Hemisensory deficit
- Unilateral neglect, apraxias
- Homonymous hemianopia or quadrantanopia
- Gaze preference with eyes deviated toward side of lesion
Posterior Cerebral Artery (PCA)
- Location: Cerebral hemisphere, posterior aspect
- Typical presentation: Cerebellar findings and visual deficits
- Symptoms:
- Visual field defects
- Vertigo
- Diplopia
- Ataxia
- Homonymous hemianopia
- Cortical blindness
- Dense sensory loss, spontaneous pain, dysesthesias, choreoathetosis
Brainstem (Posterior Cerebral Artery)
- Location: brainstem, lateral medulla
- Symptoms:
- Vertigo, nystagmus
- Horner's syndrome (miosis, ptosis, decreased sweating)
- Ataxia, falling toward side of lesion
- Impaired pain and thermal sense over half body with or without face
Brainstem (Vertebral Artery)
- Location: Brainstem, midbrain
- Symptoms:
- Third nerve palsy and contralateral hemiplegia
- Paralysis/paresis of vertical eye movement
- Convergence nystagmus
- Disorientation
Assessment
- Antiplatelet Treatment
- If on ASA already, then add Plavix (Clopidogrel) 300mg loading dose for the first day, then 75mg daily
- If no prior antiplatelet meds:
- Start ASA 325mg PO STAT, then clopidogrel
- Neuroimaging
- For any acute confusion with exertion, worry about aneurysm, repeat CT head and also do with contrast and MRI if no other focal findings
- Blood Pressure
- Maintain blood pressure: BP around 200/120 for the first 24 hours, as you want to maintain cerebral perfusion
- Further Management
- Prophylaxis for DVT
- Lower lipids
- Gradual BP reduction
Scales
- NIH Stroke Scale
Differential Diagnosis
The differential diagnosis for a stroke is broad:
- Lower motor neuron lesions (e.g., Bell's Palsy)
- Bell's Palsy = HSV infection near facial nerve
- Early corticosteroid treatment
- Ramsay Hunt = Shingles infection (VZV) near facial nerve
- Early treatment with valacyclovir prevents permanent damage
- Early corticosteroids help too
- Hypokalemia (periodic episodic paralysis)
- Episodic ataxia
- Hypoglycemia
- Electrolyte disturbance
- Tumours
- MS exacerbation
- TIA
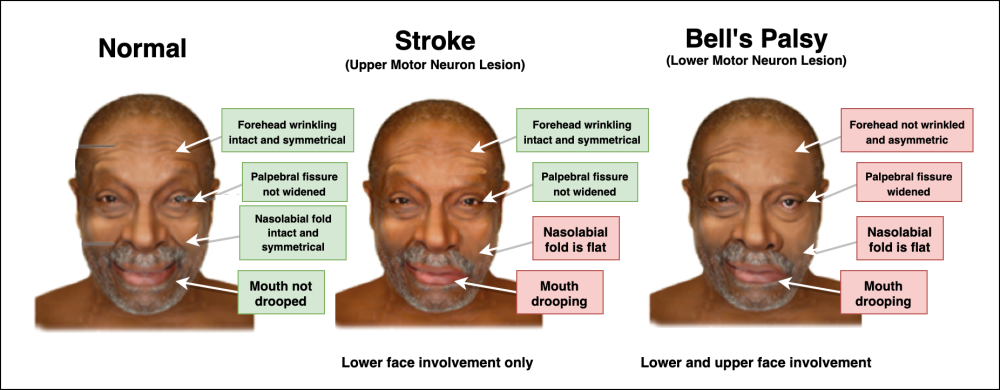
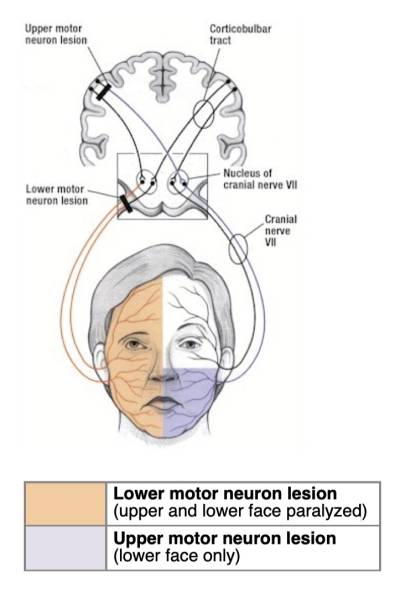
Upper Motor vs. Lower Motor Neuron Lesion
Comparison: Upper Motor Neuron Lesion vs. Lower Motor Neuron Lesion
| Normal | Upper Motor Neuron Lesion (Stroke) | Lower Motor Neuron Lesion (Bell's Palsy) | |
|---|---|---|---|
| Facial involvement | None | Lower face | Lower + upper face involvement |
| When asking patient to smile and raise eyebrows (testing CN VII) | Normal anatomic landmarks during smiling and raising the eyebrows. | • Mouth drooping • Forehead wrinkles intact | • Mouth drooping • The forehead is not wrinkled and the palpebral fissure is widened |
Comparison: Bell’s Palsy vs. Stroke
| Bell's Palsy | Acute Stroke | |
|---|---|---|
| Age | 20x-50s | > 60 |
| Onset | Hours to few days | Seconds to minutes |
| Upper face | Always affected | +/- affected |
| Lower face | Always affected | Always affected |
| Associated symptoms | Typically none | Weakness, numbness, speech difficulty, slurred speech, diplopia, swallowing difficulty, vertigo, ataxia |
Treatment
TIA
- If you're suspecting a TIA, the characteristics are:
- Symptoms are self-limiting, resolves, and goes back to baseline
- The deficits is maximal at onset, it does not get progressively worse (compared to a stroke)
- Acute onset lasting 30 mins to 1 hour
- Usually no findings on imaging
- Usually involves the MCA due to travelling of clot from ICA
- Risk factors
- Amarosis fugax, facial droop, aphasia
- Work up
- FBG, HbA1C, fasting lipid profile
- 24-hour Holter Monitor
- Clopidogrel 75mg PO daily, 300mg loading dose first
- ASA 81mg PO daily
- Insulin sliding scale if Type II Diabetes
- CT Head
Stroke (Thrombolysis)
- Treat with tPA (alteplase) within 3 hours!
- Used to be 4.5 hours? 6 hours?
- Intra-arterial tPA
- Direct local to the site of occlusion via catheter
- This gives you up to 6 hours rather than the 3 to 4.5 hours
- A lower dose can be used, and there are DECREASED systemic effects
- Then treat with aspirin after 48 hours