- Last edited on December 14, 2021
Factitious Disorder
Primer
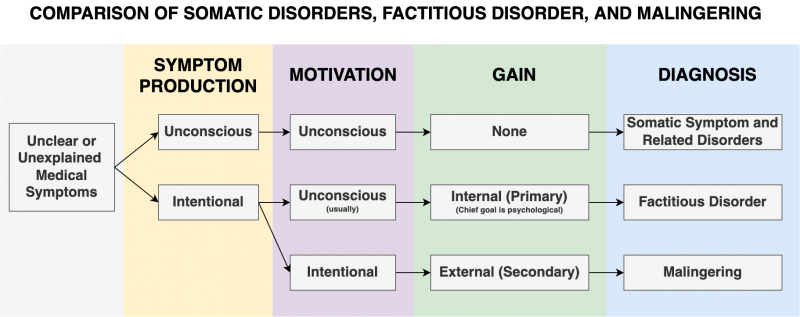
Factitious Disorder (also known as Munchausen Syndrome – named after Baron von Munchausen, an 18th-century German officer known for embellishing the stories of his life) involves the falsification of physical or psychological signs or symptoms with no obvious reward. Factitious disorder is different from hypochondriasis (an obsolete DSM-IV diagnosis) and somatic symptom disorder (now the DSM-5 diagnosis) in that patients are aware that they are exaggerating, whereas sufferers of hypochondriasis actually believe they have a disease.
Epidemiology
Prognosis
- Factitious disorder usually has first onset in early adulthood, often following a hospitalization for medical or psychiatric reasons.
- Individuals often have a history of multiple hospital admissions and are often willing to undergo invasive procedures.
- These episodes are usually intermittent; for some individuals, the pattern of behaviours can become lifelong.
- The overall prognosis is generally poor – when confronted, the majority of individuals will deny their behaviours, and very few will seek treatment.
- For factitious disorder imposed on another (FDIA), it usually begins after an initial hospitalization of the individual's child or other dependent for legitimate reasons.
- For the victims of FDIA (i.e. - children), the mortality rate can be between 6 to 22%.[5]
- Poisoning and suffocation are the most common forms of harm.
Risk Factors
- Patients may have a history of abuse or neglect as a child, experienced a true medical condition that led to extensive treatment in childhood, past important relationships with a physician, or may have underlying malicious intent towards the medical profession.
Comorbidity
- Personality disorders are common in factitious disorder.
- In factitious disorder imposed on another (FDIA), there is also high comorbidity with personality disorders, somatoform disorders, and mood disorders in the perpetrator.
DSM-5 Diagnostic Criteria
Factitious Disorder Imposed on Self
Criterion A
Falsification (i.e. - deliberately feigning) of physical or psychological signs or symptoms, or induction of injury or disease, associated with identified deception.
Criterion B
The individual presents himself or herself to others as ill, impaired, or injured.
Criterion C
The deceptive behaviour is evident even in the absence of obvious external rewards.
Criterion D
The behaviour is not better explained by another mental disorder, such as delusional disorder or another psychotic disorder.
Factitious Disorder Imposed on Another
Previously called Factitious Disorder by Proxy, or Munchausen Syndrome by Proxy.
Criterion A
Falsification of physical or psychological signs or symptoms, or induction of injury or disease, in another, associated with identified deception.
Criterion B
The individual presents another individual (victim) to others as ill, impaired, or injured.
Criterion C
The deceptive behaviour is evident even in the absence of obvious external rewards.
Criterion D
The behaviour is not better explained by another mental disorder, such as delusional disorder or another psychotic disorder.
Specifiers
Specifiers
Specify if:
- Single episode
- Recurrent episodes (
2or more events of falsification of illness and/or induction of injury)
Signs and Symptoms
- Factitious disorder requires the determination that the individual is taking surreptitious actions to deliberately misrepresent, simulate, or cause signs or symptoms of illness or injury in the absence of obvious external rewards.
- In the majority of cases of factitious disorder (both imposed on self and imposed on another), individuals present with somatic symptoms and medical disease conviction, and may exaggerate symptoms. This includes lying or faking symptoms, self-harm, or changing diagnostic tests.
- For example, there may be deceptive reports of neurological symptoms (e.g. - seizures, dizziness), manipulation of laboratory tests (e.g. - adding blood to urine tests), falsification of medical records to indicate an illness, ingestion of a substance (e.g. - insulin) to induce an abnormal laboratory result or illness (e.g. - hypoglycemia), or physically injure themselves or induce illness in themselves or another (e.g. - by injecting fecal material to cause sepsis).[6]
- There may be a dramatic but inconsistent medical history, presenting to numerous hospitals, an eagerness to have medical interventions, new symptoms following negative test results, the presence of symptoms only when the patient is alone or not being observed by a clinician, and extensive knowledge of medical terminology.[7]
- Many individuals may struggle with problems of identity and self-esteem.
Psychopathology and Pathophysiology
Differential Diagnosis
- Self-protection from liability
- Caregivers who lie about abuse injuries in dependents solely to protect themselves from liability are not diagnosed with factitious disorder imposed on another. This is because the protection from liability is an obvious external reward. Only if the deception is beyond immediate self-protection is factitious disorder imposed on another (FDIA) diagnosed.
- Early-stage medical conditions
- Clinicians suspecting factitious disorder should always rule out early-stage medical conditions.
-
- In somatic symptom disorder, there may be excessive attention and treatment seeking for perceived medical concerns, but there is no evidence that the individual is providing false information or behaving deceptively.
-
- Malingering is differentiated from factitious disorder by the intentional reporting of symptoms for personal gain (e.g. - money, time off work). In contrast, the diagnosis of factitious disorder requires the absence of obvious rewards.
- Primary (internal) gain: symptoms developed in order to assume “sick role” to get medical attention and sympathy
- Secondary (external) gain: symptoms developed for obvious external gain (e.g. - time off work, compensation)
- Conversion disorder (functional neurological symptom disorder)
- Conversion disorder is characterized by neurological symptoms that are inconsistent with neurological pathophysiology. Factitious disorder with neurological symptoms is distinguished from conversion disorder by evidence of deceptive falsification of symptoms.
-
- Deliberate physical self-harm in the absence of suicidal intent can also occur in association with other mental disorders such as borderline personality disorder. Factitious disorder requires that the induction of injury occur in association with deception.
- Medical condition or mental disorder not associated with intentional symptom falsification
- Presentation of signs and symptoms of illness that do not conform to an identifiable medical condition or mental disorder increases the likelihood of the presence of a factitious disorder. However, the diagnosis of factitious disorder does not exclude the presence of true medical condition or mental disorder, as comorbid illness often occurs in the individual along with factitious disorder. For example, individuals who might manipulate blood sugar levels to produce symptoms may also have diabetes.
Pseudologia Fantastica
Comparison of Somatic Disorders
Treatment
- The first treatment goal is to modify the individual's behaviour and reduce misuse or overuse of medical resources.
- The primary treatment for factitious disorder is psychotherapy, including psychoanalytic or psychodynamic therapy, cognitive behavioural therapy and family therapy.[8]
- Also, any underlying psychiatric disorder should be identified and treated.
- In factious disorder imposed on another, treatment considerations are similar to those in factitious disorder, with the added concern about the safety of the potential victim.
- Management often requires a team that includes social workers, foster care organizations, and law enforcement in addition to the healthcare providers.
- Involvement with the ethics department, professional regulatory bodies, and child welfare organizations is also important.