- Last edited on December 27, 2021
Hyponatremia
Primer
Hyponatremia is an electrolyte disturbance of low serum sodium that can result in neuropsychiatric symptoms. In psychiatric patients, the cause of hyponatremia is most commonly secondary to syndrome of inappropriate antidiuretic hormone secretion (SIADH) from psychotropics medications including antidepressants and antipsychotics.
Definition
Hyponatremia is defined by a serum sodium ([Na+]) concentration less than 136 mEq/L (1 mEq/L = 1 mmol/L). This indicates an excess of water relative to sodium in the extracellular fluid compartment (ECF). The normal range of serum sodium can range from 135 to 145 mEq/L.
Why does Hyponatremia Matter in Psychiatry?
Hyponatremia is frequently underdiagnosed and undertreated in both general medicine and psychiatric patients.[1] Like with other electrolyte and fluid imbalances (see also: hypokalemia, hypomagnesemia, hypocalcemia, hypercalcemia),[2] hyponatremia can cause neuropsychiatric symptoms. Acute-onset hyponatremia can cause delirium and acute behavioural changes that can be mistaken for symptoms of a psychiatric disorder. Other causes of hyponatremia, such as SIADH, may resemble psychiatric disorders or the adverse effects of psychotropic drugs, and the diagnosis of SIADH can be delayed for psychiatric patients.Approach
Hyponatremia Etiologies
| Too much water going in | Water intoxication |
|---|---|
| Too little water going out | Excessive antidiuretic hormone (ADH)* |
| Too little sodium going in | Poor IV fluid management post-operatively or general dehydration |
| Too much sodium going out | • Aldosterone or cortisol deficiency • Diuretic use • Diarrhea, burns, or vomitting |
Symptoms
Early signs and symptoms of hyponatremia includes nausea, vomiting, anorexia, disorientation, headache, fatigue, weakness, irritability, lethargy, confusion, and muscle cramps.[3] Falls and confusion in the due to hyponatremia is common in the elderly.[4] With severe hyponatremia, seizures can develop.
Etiologies
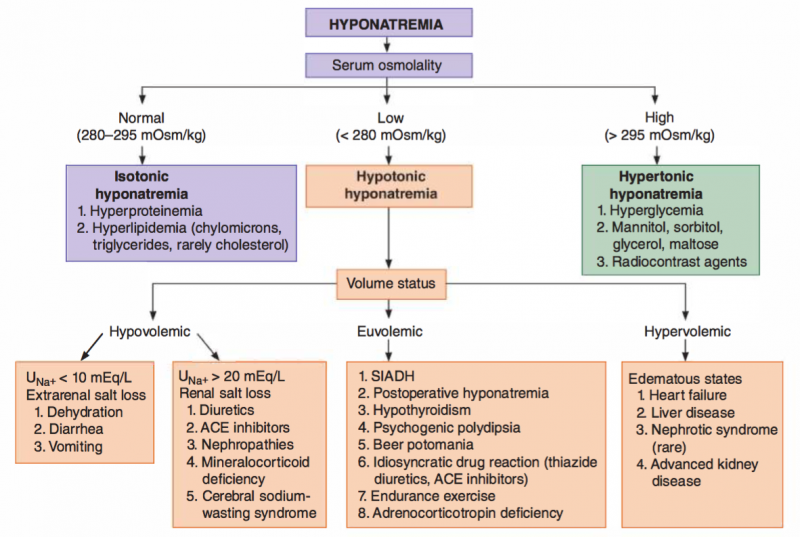
There are numerous etiologies of hyponatremia. The correct treatment and management of hyponatremia depends on identifying the etiology of the hyponatremia. For example, one must differentiate between iatrogenic hyponatremia (typically due to thiazide diuretics, carbamazepine, antidepressants, or antipsychotics), idiopathic hyponatremia, or other etiologies (like hypothyroidism or alcoholism). Generally speaking, the majority of hyponatremias in the psychiatric population are associated with physiologically inappropriate (but not necessarily elevated) levels of arginine vasopressin (AVP), leading to water retention and serum hypotonicity.
SIADH
Syndrome of inappropriate antidiuretic hormone secretion (SIADH) can cause hyponatraemia.[5] Many psychotropic medications can cause SIADH either by stimulating the release of vasopressin or by potentiating its action on the renal tubules. It is also thought that psychotropics may cause stimulation of central serotonin receptors as well. SIADH is a known side effect of antidepressants, especially in the elderly.
SIADH is characterized by the following sequence of:
- Excessive free water retention
- Euvolemic hyponatremia with continued urinary sodium excretion
- Urine osmolality > serum osmolality
Severe hyponatremia from SIADH can result in cerebral edema, and/or seizures. The treatment of SIAD consists of: (1) fluid restriction (first line), (2) salt tablets, (3) diuretics, (4) ADH antagonists, and/or (5) a slow correction of the hyponatremia with hypertonic saline to avoid osmotic demyelination syndrome (central pontine myelinolysis).
Psychogenic Polydipsia
Psychogenic polydipsia (PPD) (also known as primary polydipsia) is excessive and volitional water intake commonly patients with severe mental illness and/or developmental disability. Psychogenic polydipsia can cause hyponatremia, and is associated with minor impairments in water excretion.[6] Psychogenic Polydipsia and PIP Syndrome can be considered synonymous diagnoses.
PIP Syndrome
Psychosis, Intermittent hyponatremia, and Polydipsia Syndrome (PIP Syndrome) is a triad of symptoms observed in psychiatric patients, particularly in those with schizophrenia and/or psychosis.[7] The underlying etiology of polydipsia (compulsive water consumption) in remains unclear. Hypotheses include impairment in central thirst regulation or drug therapy, which may cause an altered sensation of thirst.[8] Usually, symptoms of this syndrome are subclinical and patients are asymptomatic. However, in severe cases, mortality can occur when the polydipsia results in severe water intoxication.[9]
Beer Potomania
Excessive consumption of beer (which has a low solute content) to the exclusion of other fluid intake can result in severe hyponatremia, known as “beer potomania.”[10]
Antidepressants
The incidence of hyponatremia caused by SSRIs varies widely, from 0.5% to 32%. In the majority of cases, hyponatremia occurs within the first 2 to 4 weeks of the onset of therapy. The hyponatremia typically resolves 2 weeks after discontinuation of the SSRI, and the incidence returns back to population baseline after 3 months.[11][12]
Hyponatremia Risk
| Higher Risk | Lower Risk |
|---|---|
| SSRIs (class effect), >5% | Mirtazapine (2.5%) |
| SNRIs (venlafaxine, duloxetine) | MAOis (moclobemide) |
| TCAs (noradrenergic ones such nortripyline, lofepramine might be safer) |
Antipsychotics
In rare cases, antipsychotics can cause hyponatremia.[13] Antipsychotics are thought to increase AVP release is increased despite normal plasma osmolality, resulting in syndrome of inappropriate antidiuretic hormone secretion (SIADH) causing hyponatremia.
Investigations
It is important to differentiate between psychotropic-induced SIADH and psychogenic polydipsia. SIADH should be a diagnosis of exclusion. To differentiate between SIADH and psychogenic polydipsia, it is important to measure serum sodium, osmolality, and urine osmolality.
Comparison
Comparison of Various Electrolyte Disturbances
| Hypo (Low Concentration) | Hyper (High Concentration) | |
|---|---|---|
| Sodium | Hyponatremia: Nausea, malaise, stupor, coma, seizures | Irritability, stupor, coma |
| Potassium | Hypokalemia: Arrhythmias, muscle cramps, spasm, and weakness. ECGs will show U waves and flattened T waves | Arrhythmias, muscle weakness. ECGs will show Wide QRS and peaked T waves. |
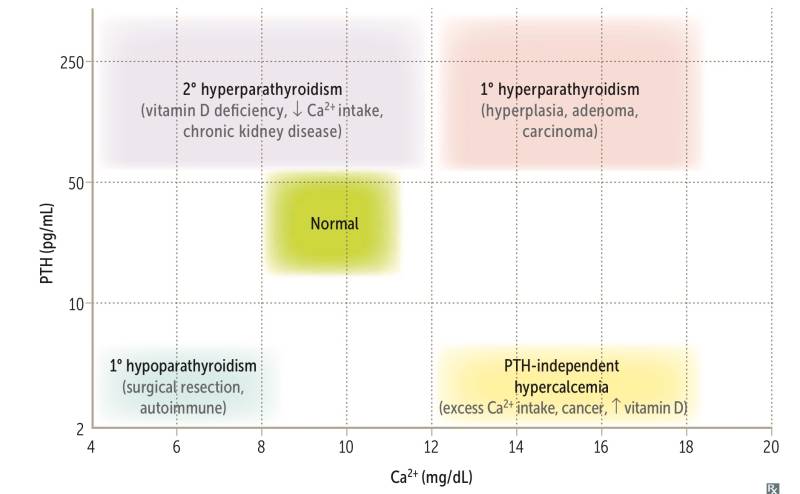
| Calcium | Hypocalcemia: Tetany, seizures, QT prolongation, twitching (e.g. - Chvostek sign), spasm (e.g. - Trousseau sign) | Hypercalcemia: Stones (renal), bones (pain), groans (abdominal pain), thrones (urinary frequency), psychiatric overtones (anxiety, altered mental status) |
| Magnesium | Hypomagnesmia: Tetany, torsades de pointes, hypokalemia, hypocalcemia | Decreased deep tendon reflexes, hypotension, lethargy, bradycardia, cardiac arrest, hypocalcemia |
| Phosphate | Bone loss, osteomalacia (adults), rickets (children) | Renal stones, metastatic calcifications, hypocalcemia |