- Last edited on July 18, 2024
Clock-Drawing Test (CDT)
Primer
The Clock-Drawing Test (CDT) is a simple and effective cognitive test used to assess executive function and visual-spatial function. It is a reliable screening tool for cognitive dysfunction, particularly for dementia. However, it lacks sensitivity for the diagnosis of early or mild dementia. The CDT can also be used to reveal neurological syndromes such as hemispatial neglect.
Download Clock Drawing Test
Indications
The CDT is useful as a quick screening cognitive test for dementia, but is generally less useful for detecting mild cognitive impairment. It tests for multiple domains of cognition, including executive function, attention, language skills, frontal lobe function, and visuospatial skills. To successfully do a clock drawing, and individual must be able to understand verbal instructions, encode instructions in short-term memory, and use visual constructive skills to draw a clock.
Neuroanatomy
- The drawing of a clock without a cue or model requires reconstructing a clock secondary to a verbal command, and having the semantic memory of a clock translated into a graphic image.
- This constructional praxis involves visuoperceptual analysis but also involves motor execution, attention, language comprehension, and numerical knowledge.[1]
- Neuroanatomical regions involved in successfully performing the CDT include both cortical and subcortical structures.
- For cortical structures, the dorsolateral prefrontal cortex, frontal, and parietal lobes are thought to be involved:
- The right parietal lobe is responsible for visual-spatial function.
- The frontal lobe and dorsolateral prefrontal cortex is responsible for planning and executive function.
- Subcortical regions including the thalamus, caudate, and corpus callosum are also involved.[2]
Instructions
Common Deficits
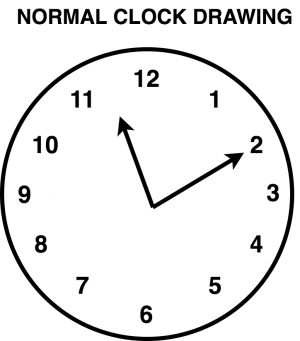
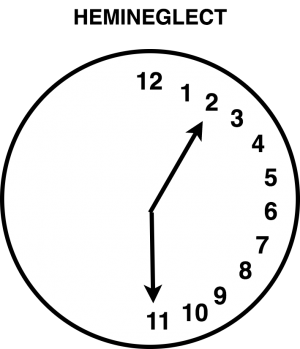
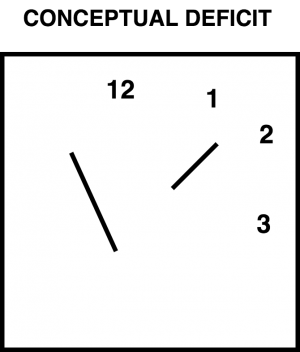
Various deficits can be seen on the clock drawing, and may be indicative of different types of dysfunction. In all examples of deficits on clock-drawing below, the instructions are for the individual to draw the clock hands at “10 past 11” (i.e. - “11:10,” with the hour hand at number “11” and the minute hand at “2.”
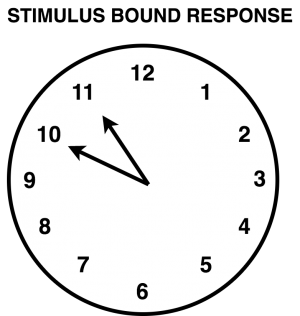
Stimulus-bound Response
The usual instructions are for the individual to set the hands of the clock to “10 after 11” or “10 past 11” (i.e. - “11:10”). If the individual instead the sets the hands at 10 and 11 (i.e. “10:55”), this indicates the individual is showing stimulus-bound behaviour. Here, the individual fails to re-code the “10” in “10 past 11” as a “2” as the minute hand on the clock. It is called stimulus bound response, because the individual is attracted to the examiner's instructions, rather than the more complex and appropriate response of re-encoding the instructions provided to them. Stimulus bound behaviours can commonly be seen in Alzheimer's disease, and is a marker for executive function deficits.[3]
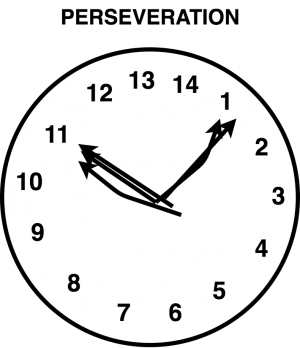
Perseveration and Pull To Stimulus
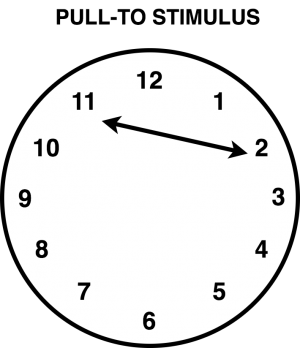
In perseveration, individuals will continue an activity despite the lack of an appropriate ongoing stimulus. For example, individuals may continue adding numbers on the clock beyond the number “12”, or draw more than two hands of the clock. Similar to stimulus-bound responses, these findings are commonly seen in dementia, and especially in Alzheimer's.[4] Another type of perseveration is a pull-to stimulus, where the individual neglects to return their hour hand back to the centre of the clock before starting a new minute hand.
Neglect and Spatial Deficits
- Neglect is the inattention to, or lack of awareness of visual space to the right or left, which can occur following damage to the processing areas of the brain.
- It should not be confused with hemianopsia, which is damage to the primary visual pathways cutting off input to the cerebral hemispheres.[5]
- In other words, neglect is a “perceptual deficit”, whereas hemianopsia is a “visual deficit”.
- Neglect can be further divided into motor and sensory components, extinction, anosognosia (denial of illness), and anosodiaphoria (minimization of illness).
- In individuals with spatial deficits, there may be crowding of numbers and/or obvious impairments in the layout of the clock.
- The usual striking example is when a clock drawing has all the numbers on one half of the clock but not the other half.
- In the example (figure 4) reveals hemineglect, the absence of numbers on the left (i.e. - left hemineglect) suggests that there is a right parietal cortical lesion. In this case, the individual would benefit from a comprehensive neurological examination.[6]
- Neglect can commonly be seen in individuals with stroke. It is most common after lesions of right parietal lobe or right frontal lobe. Other areas, such as the thalamus and the basal ganglia, can also be involved.
- Patients with right-sided lesions typically neglect the left hemispace.
- Individuals with an autoimmune encephalitis may also present with rapid cognitive impairment and deficits on clock drawing.[7]
Conceptual Deficits
In individuals with conceptual deficits, they will have a loss or impairment in the ability to retrieve knowledge about the features and/or meaning of a clock. For example, they may draw something that does not look like a clock, or draw the hour and minute hands in a way that does not actually communicate time. Conceptual deficits are thought to be due to impairments in semantic memory (i.e. - the lateral temporal lobes).[8]
Scoring and Interpretation
There are no standardized norms or scoring system for assessing the CDT. Various systems used in the literature but no one scoring system shows superior validity or predictive value. In addition to any existing neurocognitive disorder, age, educational-level, and psychiatric disorders (e.g. - depression) can also affect the clock drawing. The main aspects of the clock drawing to consider are:
- Is there correct spacing with even spaces between numbers?
- Is the placement of 3, 6, 9, and 12 correct?
- Is the placement of the clock hands (hour and minute) correct?