- Last edited on December 15, 2023
Geriatric Giants
Primer
Geriatric Giants is a term coined by geriatrician Bernard Isaacs, and the expression refers to the principal chronic disabilities of old age that impact on the physical, mental and social domains of older adults.[1] Many of these conditions, commonly misperceived to be an unavoidable part of old age, can in fact be improved. These include:
- Dementia
- Delirium
- Depression
- Incontinence
- Orthostatic Hypotension
- Falls & Dizziness
- Osteoporosis
- Polypharmacy
- Pain in the Elderly
- Failure to Thrive
- Frailty
- Elder Abuse
Attend To Your Patient's Needs First!
It is also important to make sure your patient has the appropriate care needs met to prevent them from developing the geriatric giants. These include:- Social/recreational needs (community centres, churches, religious groups)
- Medication monitoring and compliance (use blister packs and medication reminders)
- Adequate nutrition (Meals-on-Wheels)
- Assistance with housekeeping, shopping, cooking
- Caregiver education and support
- Assistance with legal matters
- Respite for caregivers
- Elder abuse issues
- Transportation
Dementia
Delirium
Depression
Incontinence
Incontinence is the involuntary loss of urine in sufficient amount or frequency to constitute a social or health problem. Even though there are aging associated changes in the bladder and the urinary tract which make the elderly person more prone to urinary incontinence, the problem is not and should not be considered as a normal part of ageing.
Orthostatic Hypotension
Orthostatic hypotension (postural hypotension) is a major and often hidden cause of falls in the elderly! Orthostatic hypotension is not a specific disease per se, rather, it is a syndrome of abnormal postural blood pressure response due to one or more underlying conditions that can affect the normal autonomic reflex arc. Orthostatic hypotension is defined as an excessive drop in blood pressure seen when changing from a lying/sitting position to assume a standing and upright posture (at least 20 mmHg systolic and/or 10 mmHg diastolic). The etiologies of the hypotension are numerous, including: hypovolemia, medications, CNS diseases, diabetes, and deconditioning.
Falls and Dizziness
- Falls are commonly in the elderly. About 30% of adults living in the community (> 65 years old) will have a fall each year. This increases to 40% in those greater than 85 years old. Nursing home residents will have an average of 1.6 falls from their beds each year. Almost half of all residents in nursing homes will have a fall more than once.
- About 12-42% of falls will result in a falls-related injury, and 20% will require medical attention.
- Individuals who have had an acute fall and hit their head should have a CT head, according to the Focused Falls Decision Rule, to rule out intracranial bleeds.[2]
- 10% of falls will result in a fracture, of which 25% are hip fractures, which have a 20% mortality rate within 1 year.
- Long term, falls result in increased disability, functional decline, loss of independence, reduced quality of life, fears of falling, depression, and social isolation.
Falls Risk Factors
Adapted from: Public Health Agency of Canada. Seniors’ Falls in Canada: Second Report. 2014| Biological | Behavioural | Socioeconomic | Environmental | |
|---|---|---|---|---|
| Risk Factors | • Age • Gender (females > males) • Acute illness • Balance and gait deficits • Chronic conditions and medical co-morbidity • Chronic disability • Cognitive impairment • Vision impairment • Muscle weakness • Reduced fitness | • Alcohol • Fear of falling • Inappropriate assistive device • Inappropriate footwear and clothing • Falls history • Poor nutrition and hydration • Medications • Risk taking behaviour • Vitamin D | • Living alone • Poor living conditions • Lack of social supports • Lack of transportation • Low education • Literacy • Language barriers | • Stairs • Home hazards • Lack of home equipment • Obstacles • Tripping hazards • Slippery or uneven surface • Inadequate building codes • Community design • Building maintenance • Footwear • Winter weather |
Management of falls requires a multifactorial approach including:
- A multifactorial risk assessment and comprehensive management
- A comprehensive history
- Cognition and assessment of function
- Physical exam (especially orthostatic vitals)
- Home occupational therapy (OT) safety assessment
- Exercise, or other forms of physical activity such as tai chi
- Vitamin D supplementation is possibly helpful, especially in individuals with low vitamin D
- Vision (removing cataracts
- Medication review (Highest risk: psychotropics, anticholinergics, and antihypertensives)
- Gait aids (cane, walker, wheelchair)
Medications
Changes in pharmacokinetics and pharmacodynamics occur with aging in relation to many drugs, resulting in delayed elimination and increased bioavailability, which increases the risk for falls due to orthostatic hypotension. Additionally, beta-adrenergic receptor responsiveness is decreased in the elderly.[3]
Polypharmacy
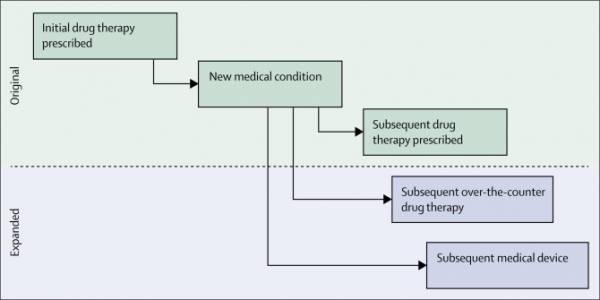
Polypharmacy is a major health issue for elderly populations. A majority of the elderly (>65 years) take more than 5 medications. Geriatic patients experience major changes in pharmacodynamics and pharmacokinetics that affect how medications work. Polypharmacy can often resulting prescribing cascades (figure 1), where a drug is prescribed, an adverse drug event occurs that is misinterpreted as a new medical condition, and a subsequent drug is prescribed to treat this drug-induced adverse event.[4]
Beer's List
Beer's List is a list of medications that should be avoided in the elderly due to the propensity to cause sedation, falls, and anticholinergic side effects. Benzodiazepines in particular causes daytime sedation, motor vehicle accidents, falls/fractures, cognitive decline, and physical dependence. Avoid using benzodiazepines if at all possible, and if absolutely needed, use the lowest effective dose, with a goal for reassessment and taper. Short/intermediate acting benzodiazepines should also be used over long-acting ones.
STOPP/START
Screening Tool of Older Person's Prescriptions (STOPP) and Screening Tools to Alert Doctors to Right Treatment (START) is a medication review tool designed to identify medications where the risks outweigh the benefits in the elderly.
Pain
Pain increases in incidence and prevalence after age 60. This is because of the accumulative burden of aging-associated illnesses such as osteoarthritis, compression fractures, diabetic neuropathy, and cancer. It is underreported by the elderly. The most common causes of pain is osteoarthritis (close to 50%).
Osteoporosis
Osteoporosis is progressive low bone mass & micro-architectural deterioration that leads to skeletal weakness and an increased risk of bone fracture; specifically it is a Bone Mineral Density (BMD) T-score of 2.5 or less (which is the equivalent of a bone density lower than 648mg/cm2). Osteoporosis can be primary (a combinational of post-menopasual loss of estrogen in females, and/or related to aging losses of osteoblasts seen in both men and women) or secondary to some other disorder (such as osteomalacia, hyperparathyroidism, hyperthyroidism, glucocorticoid excess, renal failure, liver disease, etc.).
Frailty
Frailty is the clinical presentation of cumulative biologic changes with aging which result in decreased ability to maintain homeostasis and lead to vulnerability to stressors.[5] Fragility can be measured via certain clinical scales, such as the Rockwood Clinical Frailty Scale (Clinical Frailty Scale).
Rating Scales for Frailty
| Name | Rater | Description | Download |
|---|---|---|---|
| Clinical Frailty Scale (CFS) | Clinician | An inclusive 9-point scale introduced to summarize the overall level of fitness or frailty of an older adult after they have been evaluated by a health care professional. | Download |
Failure to Thrive
Failure to Thrive (FTT) is a syndrome of weight loss, decreased appetite, poor nutrition and inactivity, often accompanied by dehydration, depressive symptoms, impaired immune function and low cholesterol. A work up of FTT requires an interdisciplinary and comprehensive assessment.
Elder Abuse
Elder abuse is defined as any action or inaction that threatens the well being of an older person. Abuse can take many forms, but is usually grouped in 4 major categories: (1) physical/sexual abuse, (2) emotional/psychological abuse, (3) financial abuse (this is the most common), (4) neglect.