- Last edited on January 7, 2022
Introduction to the Autonomic Nervous System
Primer
The Autonomic Nervous System (ANS) plays a significant role in unconscious and automatic processes in the human body. As prescribers of medications, what you prescribe can have profound impacts on the ANS, and it is important to be aware of how and why medications affect the ANS.
The Nervous System
Central and Peripheral Nervous System
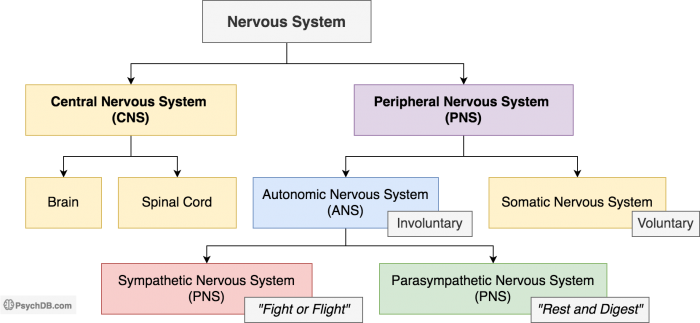
The nervous system can be broken down into:
- Central Nervous System (CNS), your brain and spinal cord
- Peripheral Nervous System (PNS), which consists of:
- (1) Sensory Division, sensory neurons which transmit signals from receptors to the CNS
- (2) Motor Division, motor neurons which transits signals from the CNS to receptors.
- This division includes the Autonomic Nervous System (ANS), which is responsible for involuntary responses, and the Somatic Nervous System, which controls voluntary movement
Autonomic Nervous System (ANS)
The Autonomic Nervous System (ANS) operates independently of the CNS (e.g. - you do not need to consciously tell your heart to beat faster when you run). However, the ANS can be influenced by the brain (e.g. - salivating at the smell of food).
The Autonomic Nervous System (ANS) has 2 parts:
- Sympathetic Nervous System (SNS), also known as the “Fight-or-Flight” system
- Parasympathetic Nervous System (also called the PNS), usually (but not always!) causes the opposite effect of the SNS, also known as the “Rest-and-Digest” System
Anatomy 101
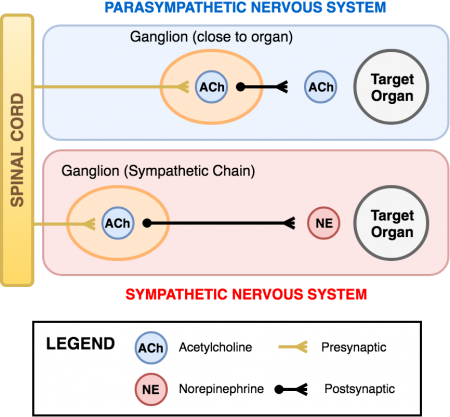
The Sympathetic and Parasympathetic Nervous Systems exit the brain and spinal cord and enter “relay stations” known as a ganglion. The parasympathetic ganglia are located close to the organs they innervate. Sympathetic ganglia, on the other hand, are in the sympathetic chain (which runs along the spinal column) and are far away from the organs (see figure 1). Messages from the brain pass from the preganglionic neuron, through the ganglion, to the postganglionic neuron, and finally to the target organ.
Acetylcholine (Ach)
Acetylcholine (Ach) is the “preganglionic nerve to ganglion to postganglionic nerve” neurotransmitter for both the sympathetic and parasympathetic systems. Acetylcholine is also the “postganglionic nerve to organ” neurotransmitter for the parasympathetic system (PNS)
Norepinephrine (NE)
Norepinephrine (NE) is the “postganglionic nerve to organ” neurotransmitter for the sympathetic system (SNS)
Summary
So which neurotransmitter binds onto which receptor on the autonomic pathway?
Neurotransmitters and Receptors
| Neurotransmitter | Acetylcholine (ACh) | Norepinephrine (NE), Epinephrine (E) |
|---|---|---|
| Preganglionic neuron (SNS/PNS) | - | |
| Ganglion (SNS/PNS) | - | |
| Postganglionic neuron (SNS/PNS) | - | |
| Postganglionic nerve to organ (PNS) | - | |
| Postganglionic nerve to organ (SNS) | - | |
| Receptor | Muscarinic (M) and nicotinic (N) receptors | Alpha (α) and beta (β) receptors |
| Receptor Subtype Examples | M1, M2, M3 | α1, α2, β1, β2 |
These Receptors Exist Outside the ANS Too!
Don't forget all of these receptors in the ANS exist elsewhere too. Like: nicotinic receptors in the addiction pathway, nicotine receptors in the neuromuscular junction, mediating skeletal muscle innervation, muscarinic receptors in the brain involved in Parkinson’s disease and movement disorders.Interesting Exceptions
- There is no parasympathetic innervation of blood vessels
- Sweat glands are innervated by sympathetic nerves, but paradoxically use M receptors
- Sexual arousal is parasympathetic but orgasm is sympathetic
- The sympathetic innervation of the adrenal gland is directly from the spinal cord and uses acetylcholine as the neurotransmitter. The adrenal gland functions like a special form of ganglion which then secretes epinephrine directly into the bloodstream.
Sympathetic Receptors
Alpha (α)
The following table details the function and location of sympathetic receptors, as well as example agonists and antagonists.
Alpha (α)Receptor Function and Location
| Receptor | Neurotransmitter | Receptor Type | Function | Location | Agonist | Antagonist |
|---|---|---|---|---|---|---|
| Alpha-1 (α1) | Norepinephrine | G-protein | Constriction of smooth muscles | • Blood vessels and skin piloerectors (vasoconstriction and goosebumps) • Sphincters (bladder, GI) • Uterus (contraction) • Eye (constriction of radial muscle, leading to pupillary dilation (mydriasis) | • Epinephrine • Phenylephrine • Midodrine | • Prazosin (antihypertensive) • Tamsulosin • Terazosin • Trazodone (blockade can cause priapism) • Antipsychotics (α1-blockade can cause orthostatic hypotension) |
| Alpha-2 (α2) | Norepinephrine | G-protein | Inhibition of the sympathetic ganglia (i.e. - decreasing SNS activity) | • Presynaptic ganglionic neurons • GI tract | • Clonidine, guanfacine (antihypertensive, helps with ADHD, tics) | • Mirtazapine, trazodone (antidepressant effect) |
Alpha Agonists and Antagonists
| Agonist | Non selective blocker | Selective blocker (-osin ending) | |
|---|---|---|---|
| α1 | • Epinephrine • Phenylephrine • Midodrine | • Phenoxybenzamine • Phentolamine | • Prazosin • Terazosin • Doxazosin • Tamsulosin |
| α2 | • Clonidine • Guanfacine | • Phenoxybenzamine • Phentolamine | • Mirtazapine |
Beta (β)
Beta (β) Receptor Function and Location
| Receptor | Function | Location | Agonist | Antagonist |
|---|---|---|---|---|
| Beta-1 (β1) | Increases cardiac performance, liberation of energy, and conservation of water | • Heart • Fat cells (lipolysis) • Kidneys (releases renin to conserve water) | • Dobutamine (used as a positive inotrope for heart failure and cardiogenic shock) | • Atenolol • Bisporolol (selective β1 receptor antagonist) • Metoporolol (selective β1 receptor antagonist) • Propranolol (β1- and β2-adrenergic receptor antagonist) |
| Beta-2 (β2) | Relaxation of smooth muscles (e.g. in the lungs), and liberation of energy | • Lungs (bronchodilation) • Blood vessels in muscles (vasodilation) • uterus (uterine relaxation) • GI (intestinal relaxation) • Bladder (relaxation) • Liver (liberate glucose via glycogenolysis) | • Salbutamol [AKA Albuterol] (Short-acting β2 agonist, SABA) • Formoterol (Long-acting β2 agonist (LABA) | • Propranolol (β1- and β2-adrenergic receptor antagonist) |
β1-selective antagonists (β1 > β2)
- acebutolol (partial agonist)
- atenolol
- bisoprolol
- metoprolol
Nonselective antagonists (β1 = β2)
- nadolol
- pindolol (partial agonist)
- propranolol
- timolol
Modulating Sympathetic Activity
Most of the time, the SNS and PNS are opposing each other. Therefore, to change this balance, one system can be strengthened, or the other weakened.
Modulating Sympathetic Activity
| To increase (↑) sympathetic activity | To decrease (↓) sympathetic activity |
|---|---|
You want to increase stimulation of the α and β receptors:
| You want to decrease stimulation of the α and β receptors:
|
Parasympathetic Receptors
The following table details the function and location of parasympathetic receptors, as well as example agonists and antagonists.
Muscarinic (M) and Nicotinic (N)
Muscarinic (M) and Nicotinic (N) Receptor Function and Location
| Receptor | Function | Location | Agonist | Antagonist |
|---|---|---|---|---|
| Nicotinic (N) | “Nerve to nerve” and “nerve to muscle” communication | • Sympathetic and parasympathetic ganglia • Neuromuscular junction (NMJ) | • Nicotine • Varenicline • Succinylcholine (indirect anticholinergic)* | • Pancuronium • Vecuronium |
| Muscarinic (M) | Opposes most sympathetic actions at the level of the organs | • Lungs (bronchoconstriction) • Heart (bradycardia, decreased conduction, decreased contractility) • Sphincters of GI and bladder (relaxes) • Bladder wall (constriction) • GI (intestinal contraction) • Eye (contraction of the circular muscle = pupilary constriction/miosis) • Eye (contraction of the ciliary muscle = focus for near vision) • Glands: lacrimal, salivary, bronchial (secretions) | • Pilocarpine (stimulates secretion of large amounts of saliva and sweat, and increases aqueous humour turnover in open angle glaucoma) • Methacholine | • Atropine (non-selective antagonism), causes tachycardia • Benztropine (selective M1 muscarinic receptor antagonist) • Ipratropium (non-selective antagonism), bronchodilation • Tiotropium (non-selective antagonism), bronchodilation • Scopolamine • Hydroxyzine • Diphenhydramine “Benadryl” (non-selective antagonism) • Dimenhydrinate “Gravol” • Oxybutynin • Procyclidine (non-selective antagonism), for idiopathic or drug-induced Parkinson's |
How Does Succinylcholine Work?
Succinylcholine is a direct nicotinic receptor agonist but is used clinically as an indirect anticholinergic. It is a direct cholinergic agonist because it binds to the same binding site as acetylcholine and activates the receptor in the same manner. However, unlike endogenous acetylcholine, succinylcholine activates the nicotinic receptors so intensely that a depolarizing block occurs immediately followed by a desensitizing block (think of the phases of the action potential). This is what gives succinylcholine its paralyzing (i.e. - muscle relaxant) effects in anesthesia. In contrast, non-depolarising neuromuscular blocking agents (NMBAs), such as pancuronium, are direct cholinergic antagonists.Muscarinic Subtypes
Muscarinic Subtypes
| Muscarinic Receptor Subtype | Location | Description |
|---|---|---|
| M1 | Central nervous system | Involved in perception, attention, and cognition. Delirium is also associated with the antagonism of post-synaptic M1 receptors. |
| M2 | Brain, heart | Decreases heart rate below baseline normal sinus rhythm by slowing the speed of depolarization. |
| M3 | Smooth muscles, salivary glands | Causes contraction of smooth muscle, including bronchoconstriction and bladder voiding. |
| M4 | Brain, lungs, salivary glands | There is a possible role for M4 receptors in regulating salivary protein secretion. Agonism of M4 is thought to be involved in clozapine-induced sialorrhea. |
Modulating Parasympathetic Activity
Most of the time, the SNS and PNS are opposing each other. Therefore, to change this balance, one system can be strengthened, or the other weakened.
Modulating Parasympathetic Activity
| To increase (↑) parasympathetic activity | To decrease (↓) parasympathetic activity |
|---|---|
| You want to increase stimulation of the M (and N) receptors: • Give a muscarinic (M) agonist (AKA cholinergic - also called a vagotonic, since the vagus nerve is the primary PNS nerve) • Inhibit the breakdown or removal of endogenous acetylcholine (e.g. - acetylcholinesterase inhibitor such as physostigmine) | You want to decrease stimulation of the M (and N) receptors: • Give a muscarinic (M) antagonist (AKA anticholinergic or parasympatholytic) (e.g. - atropine to increase heart rate) |