- Last edited on January 3, 2022
Introduction to Neurotransmitters and Receptors
Primer
Understanding Neurotransmitters and Receptors is important due to the frequent use of psychotropic medications in psychiatry.
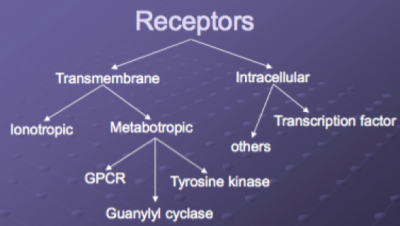
Receptors
Evolution of Neuroceptors
The dopamine, muscarinic, adrenergic, serotonin, opiate, and histamine receptors are all evolutionarily related to a common ancestor.
G-protein coupled receptors
- Muscarinic acetylcholine receptors
- Adenosine, Rhodopsin
- GABAB, Adrenergic receptors
- Cannabinoid, Opioid
- Cholecystokinin, Glucagon, Secretin, Somatostatin
- Dopamine, Serotonin (except 5-HT3) Metabotropic glutamate receptors Histamine, Olfactory receptors
Ionotropic receptors
- Nicotinic acetylcholine
- Glycine (GlyR)
- GABAA, GABAC
- Glutamate: NMDA, AMPA, Kainate
- 5-HT3 (Serotonin)
Neurotransmitter Changes Associated with Diseases/Disorders
| Dopamine | Serotonin | Acetylcholine | Norepinephrine | GABA | |
|---|---|---|---|---|---|
| Alzheimer's disease | - | - | ↓ | - | - |
| Anxiety | - | ↓ | - | ↑ | ↓ |
| Schizophrenia | ↑ (excess dopamine causes positive symptoms and psychosis) | - | - | - | - |
| Depression | ↓ | ↓ | - | ↓ | - |
| Huntington's disease | ↑ | - | ↓ | - | ↓ |
| Parkinson's disease | ↓ (destruction of dopamine-producing substantia nigra) | ↓ | ↑ (cholinergic excess causes Parkinsonism) | - | - |
Neurotransmitters
Neurotransmitters can be inhibitory (which reduces neuronal excitability), or be excitatory (which increases neuronal excitability). Inhibitory and excitatory action will decrease or increase, respectively, the likelihood that a neuron will fire an action potential.
Types
- Monoamine Family
- Catecholamines
- Tyrosine
- L-DOPA
- Dopamine
- Norepinephrine
- Epinephrine
- Indolamines
- Serotonin
- Melatonin
- Trimonoaminergic neurotransmitter system
- Norepinephrine (NE)
- Dopamine (DA)
- Serotonin (5-HT)
Monoamine Processing
- Degradation
- Monoamine Oxidases A & B (MAO-A and MAO-B) in mitochondria of presynaptic neuron and elsewhere
- Catechol-O-methyl-transferase (COMT) outside of the presynaptic nerve terminal
- Reuptake
- Transport pumps (NET, SERT, DAT)
Serotonin
- Serotonin is produced in presynaptic neurons by hydroxylation and decarboxylation of l-tryptophan. Serotonin is then incorporated into vesicles, where it resides until it is needed for neurotransmission. After axonal stimulation, serotonin is released into the intrasynaptic space; presynaptic serotonin receptors function as a feedback loop to inhibit exocytosis of vesicles. Serotonin then binds to postsynaptic receptors to effect neurotransmission. A reuptake mechanism returns serotonin to the cytoplasm of the presynaptic neuron, where it is reintroduced into vesicles. Serotonin is then metabolized by monoamine oxidase subtype A to hydroxyindoleacetic acid.
- Serotonin receptors are divided into seven 5-hydroxytryptamine (5-HT) families (5-HT1 to 5-HT7), several of which have multiple members (e.g. - 5-HT1A, 5-HT1B, 5-HT1C, 5-HT1D, 5-HT1E, and 5-HT1F). Further structural and operational diversity is achieved by allelic polymorphisms, splice variants, receptor isoforms, and the formation of receptor heterodimers.
- Serotonergic neurons in the CNS are found primarily in the midline raphe nuclei, located in the brain stem from the midbrain to the medulla. The rostral end of this system is involved in the regulation of wakefulness, affective behavior, food intake, thermoregulation, migraine, emesis, and sexual behavior. The neurons of the raphe in the lower pons and medulla participate in the regulation of pain nociception and motor tone. In the periphery, the serotonin system regulates vascular tone and gastrointestinal motility.
Serotonin Receptor Agonists, Partial Agonists, and Antagonists
| Serotonin Receptor | Neurotransmitter | Receptory Type | Agonist | Partial Agonist | Antagonist |
|---|---|---|---|---|---|
| 5-HT1 | Serotonin | G-protein coupled | • Mirtazapine (antidepressant effect) | - | Unknown downstream effects |
| 5-HT1A | Serotonin | G-protein coupled | Buspirone (anti-anxiety effects) | Anxiolytic (buspirone); booster of antidepressant action (aripiprazole) | - |
| 5-HT2A | Serotonin | G-protein coupled | Sexual dysfunction, insomnia, anxiety (SSRIs) | - | • Possible mood stabilizing and antidepressant actions in bipolar disorder (atypical antipsychotics) • Reduction of sexual dysfunction (trazodone, aripiprazole, cyproheptadine) • Reducing motor side effects from serotonin syndrome (cyproheptadine) • Mirtazapine (antidepressant effect) |
| 5-HT2C | Serotonin | G-protein coupled | Sexual dysfunction (SSRIs) | - | • Mirtazapine (antidepressant effect) |
| 5-HT3 | Serotonin | Ligand-gated ion channel (the only serotonin receptor one!) | • Not involved in psychiatric symptoms • These receptors do one thing mainly, and they do it well: when they stimulated (i.e. - targeted by an agonist) they make you really nauseous - if patients report nausea on an SSRI, this is why! | - | • Anti-nausea (mirtazapine,olanzapine, and ondansetron are all 5-HT3 antagonists) • Used in cancer populations for chemotherapy-related nausea |
| 5-HT4 | Serotonin | G-protein coupled | Increased GI motility, peristalsis, increase gastric emptying | - | - |
Dopamine
- Concentrations of dopamine are highest in the caudate (with dopaminergic neurons projections from the substantia nigra)[1]
Dopamine Receptor Agonists, Partial Agonists, and Antagonists
| Dopamine Receptor | Neurotransmitter | Receptor Type | Agonist | Partial Agonist | Antagonist |
|---|---|---|---|---|---|
| D2 | Dopamine | G-protein coupled | L-dopa | Aripiprazole (partial agonist) creates an antipsychotic effect. | Typical and atypical antipsychotics create an antipsychotic effect. |
Acetylcholine
- Acetylcholine is a fundamental neurotransmitter used throughout the body: at the neuromuscular junction, in the autonomic nervous system (both sympathetic and parasympathetic), and finally, in the brain for neuromodulation of arousal, attention, memory and motivation. There are two different acetylcholine (ACh) receptor types: muscarinic (M) receptors, and nicotinic (N).
- Acetylcholine is stored in vesicles in the terminal portions of nerves. It gets released when an action potential is conducted through the neuron and opens up calcium (Ca) channels that allows calcium to enter the neuron. Calcium causes binding of the Ach vesicles to the presynaptic membrane, after which Ach is released into the synaptic cleft.
Muscarinic (Acetylcholine) and Nicotinic Receptor Agonists, Partial Agonists, and Antagonists
| Receptor | Neurotransmitter | Receptor Type | Location | Function | Agonist | Partial Agonist | Antagonist |
|---|---|---|---|---|---|---|---|
| M1 | Acetylcholine | G-protein receptor | Central nervous system | Involved in perception, attention, and cognition. | Experimental drugs only | - | Many antipsychotics, and antidepressants can cause the anticholinergic effects of memory disturbance, sedation, dry mouth, blurred vision, constipation, urinary retention. Delirium is also associated with the antagonism of post-synaptic M1 receptors. |
| M2 | Acetylcholine | G-protein receptor | Brain, heart | Decreases heart rate below baseline normal sinus rhythm by slowing the speed of depolarization. | - | - | - |
| M3 | Acetylcholine | G-protein receptor | Smooth muscles, salivary glands | Causes contraction of smooth muscle, including bronchoconstriction and bladder voiding. | - | - | - |
| M4 | Acetylcholine | G-protein receptor | Brain, lungs, salivary glands | There is a possible role for M4 receptors in regulating salivary protein secretion. Agonism of M4 is thought to be involved in clozapine-induced sialorrhea. | - | - | - |
| M5 | Acetylcholine | G-protein receptor | Smooth muscles, salivary glands | - | - | - | May contribute to metabolic syndrome (dyslipidemia and diabetes), from some atypical antipsychotics |
Breakdown
In the synaptic cleft, acetylcholine binds to M or N receptors. Once in the cleft, ACh has 3 fates:
- It is broken down by acetylcholinesterase (most important)
- It is taken back (reuptake) into the presynaptic neuron
- It diffuses away out of the synaptic cleft
Terminology Reminder
- Muscarinic Antagonists = Anticholinergics = Antimuscarinics = Vagolytics (think atropine, benztropine, diphenhydramine, scopolamine)
- Muscarinic Agonists = Cholinergics = Muscarinics = Vagotonics
Modulation
Acetylcholine activity can be modulated with 3 different classes of drugs:
- Muscarinic Agonists (increase PNS activity)
- Used to cause constriction of the pupil (pilocarpine) or to promote salivation for dry mouth (cevimeline)
- Muscarinic Antagonist (Anticholinergic) (decrease PNS activity)
- Dilates the pupil, decrease oral secretions (glycopyrrolate), increases the heart rate (atropine), dilates bronchioles (ipratropium), treats incontinence/spasms of the bladder (tolteridine), relaxes GI spasms, treats movement disorders such as Parkinson’s Disease and Tardive Dyskinesia (benztropine), treat poisonings from insecticide or chemical warfare (atropine)
- Acetylcholinesterase Inhibitors (increase PNS activity)
- Also known as Cholinesterase inhibitors
- Donepezil, galantamine, rivastigmine for Alzheimer's dementia
- Neostigmine for myasthenia gravis
- Physostigmine for glaucoma, GHB intoxication
Norepinephrine
Adrenergic agonists include:
- Mixed receptor drugs (α and β agonists):
- epinephrine
- norepinephrine (nor = no radical = no CHx group)
- dopamine
- Pure α1
- phenylephrine
- Pure β1
- Isoproterenol
Adrenergic antagonists include:
- Beta blockers (β antagonists)
- -olol drugs (e.g. metoprolol)
- Alpha blockers (α1 antagonists)
Glutamate
- Glutamate is the main excitatory neurotransmitter in the brain, and acts on NMDA receptors. Ketamine is an example of an NMDA receptor antagonist.
Histamine
- Histamine is an organic nitrogenous compound involved in local immune responses, regulation of physiological function in the gut and also as a neurotransmitter in the brain, spinal cord, and uterus. Histamine exerts its effects primarily by binding to G protein-coupled histamine receptors (subtypes: H1, H2, H3, H4). Antihistamine medications block or reduce histamine-mediated effects at one of four identified histamine receptors.
Histamine Receptor Functions and Locations
| Histamine Receptor Subtype | Neurotransmitter | Receptor Type | Function | Location | Agonists | Antagonists/Blocker |
|---|---|---|---|---|---|---|
| H1 | Histamine | G-protein | Allergic responses | Smooth muscle and endothelial cells | Hydroxyzine (inverse agonist - acts like an antagonist), Betahistine (H1 agonist) | • First-generation: Diphenhydramine • Second-generation: Loratadine, cetirizine Therapeutic effect for anxiety and insomnia; side effect of sedation and weight gain Also trazodone |
| H2 | Histamine | G-protein | Stimulation of gastric acid | Gastric parietal cells | Betazole (H2 agonist - stimulates gastric secretions) | Ranitidine |
| H3 | Histamine | G-protein | Release of neurotransmitters including histamine, acetylcholine, dopamine, norepinephrine, and others involved in cognition | Presynaptic receptors in central nervous system | None | Betahistine |
| H4 | Histamine | G-protein | Inflammatory responses | Hematopoietic cells such as eosinophils, mast cells, neutrophils, and dendritic cells | None | None |
What are Antihistamines?
The term “antihistamine” is generally used to describe a medication that antagonizes histamine activity at H1 receptors.- First-generation antihistamines such as diphenhydramine are widely available without a prescription and commonly used to treat allergic symptoms. They are sedating as the cross the blood-brain barrier. First-generation antihistamines are often are used in cold/cough medications and over-the-counter (OTC) sleep aid medications due to their sedating effect.
- Second-generation antihistamines are less likely to cross the blood-brain barrier than first-generation antihistamines, and thus less have central nervous system effects, such as drowsiness. Second-generation antihistamines include loratadine and cetirizine.[2]
GABA
- GABA (γ-aminobutyric acid) is the most common neurotransmitter in the CNS. It is also the main inhibitory neurotransmitter in the brain and central nervous system. High concentrations are found in the cortex and limbic system. It is one of the key neurotransmitters involved in anxiety.
- There are 3 major types of GABA receptors (A, B, and C) and numerous subtypes. GABA-A and GABA-C receptors are both ligand-gated ion channels and are part of a complex that forms an inhibitory chloride channel.
- GABAA receptors are targets of benzodiazepines, sedative hypnotics, barbiturates, and/or alcohol, and are involved with either tonic or phasic inhibitory neurotransmission at GABA synapses.
- GABAB receptors have a different receptor class, namely, G-protein-linked receptors. GABAB receptors may be coupled to calcium and/ or potassium channels, and may be involved in pain, memory, mood, and other CNS functions.