- Last edited on April 30, 2020
Introduction to the Autonomic Nervous System
Primer
The Autonomic Nervous System (ANS) plays a significant role in unconscious and automatic processes in the human body. As prescribers of medications, what you prescribe can have profound impacts on the ANS, and it is important to be aware of how and why medications affect the ANS.
The Nervous System
Central and Peripheral Nervous System
Before we talk about the effects of anticholinergics/cholinergics, we need to review briefly the anatomical structures that these drugs affect. They primarily (but not exclusively) affect the nervous system.
The nervous system can be broken down into:
- Central Nervous System (CNS), your brain and spinal cord
- Peripheral Nervous System (PNS), which consists of:
- (1) Sensory Division, sensory neurons which transmit signals from receptors to the CNS
- (2) Motor Division, motor neurons which transits signals from the CNS to receptors.
- This division includes the Autonomic Nervous System (ANS), which is responsible for involuntary responses, and the Somatic Nervous System, which controls voluntary movement
Autonomic Nervous System (ANS)
The Autonomic Nervous System (ANS) operates independently of the CNS (e.g. - you do not need to consciously tell your heart to beat faster when you run). However, the ANS can be influenced by the brain (e.g. - salivating at the smell of food).
The Autonomic Nervous System (ANS) has 2 parts:
- Sympathetic Nervous System (SNS), also known as the “Fight-or-Flight” system
- Parasympathetic Nervous System (also called the PNS), usually (but not always!) causes the opposite effect of the SNS, also known as the “Rest-and-Digest” System
Anatomy 101
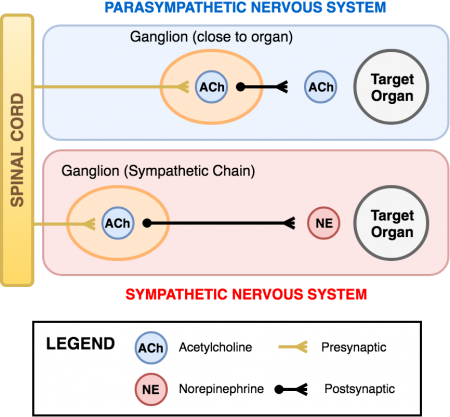
The Sympathetic and Parasympathetic Nervous Systems exit the brain and spinal cord and enter “relay stations” known as a ganglion. The parasympathetic ganglia are located close to the organs they innervate. Sympathetic ganglia, on the other hand, are in the sympathetic chain (which runs along the spinal column) and are far away from the organs (see figure 1). Messages from the brain pass from the preganglionic neuron, through the ganglion, to the postganglionic neuron, and finally to the target organ.
Acetylcholine (Ach)
Acetylcholine (Ach) is the “preganglionic nerve to ganglion to postganglionic nerve” neurotransmitter for both the sympathetic and parasympathetic systems. Acetylcholine is also the “postganglionic nerve to organ” neurotransmitter for the parasympathetic system (PNS)
Norepinephrine (NE)
Norepinephrine (NE) is the “postganglionic nerve to organ” neurotransmitter for the sympathetic system (SNS)
Summary
So which neurotransmitter binds onto which receptor on the autonomic pathway?
Neurotransmitters and Receptors
| Neurotransmitter | Acetylcholine (ACh) | Norepinephrine (NE), Epinephrine (E) |
|---|---|---|
| Preganglionic neuron (SNS/PNS) | - | |
| Ganglion (SNS/PNS) | - | |
| Postganglionic neuron (SNS/PNS) | - | |
| Postganglionic nerve to organ (PNS) | - | |
| Postganglionic nerve to organ (SNS) | - | |
| Receptor | Muscarinic (M) and nicotinic (N) receptors | Alpha (α) and beta (β) receptors |
| Receptor Subtype Examples | M1, M2, M3 | α1, α2, β1, β2 |
These Receptors Exist Outside the ANS Too!
Don't forget all of these receptors in the ANS exist elsewhere too. Like: nicotinic receptors in the addiction pathway, nicotine receptors in the neuromuscular junction, mediating skeletal muscle innervation, muscarinic receptors in the brain involved in Parkinson’s disease and movement disorders.Interesting Exceptions
- There is no parasympathetic innervation of blood vessels
- Sweat glands are innervated by sympathetic nerves, but paradoxically use M receptors
- Sexual arousal is parasympathetic but orgasm is sympathetic
- The sympathetic innervation of the adrenal gland is directly from the spinal cord and uses acetylcholine as the neurotransmitter. The adrenal gland functions like a special form of ganglion which then secretes epinephrine directly into the bloodstream.
Sympathetic Receptors
Alpha (α) and Beta (β)
The following table details the function and location of sympathetic receptors, as well as example agonists and antagonists.
Learn this table and you will learn to better care for your patients!
Alpha (α) and Beta (β) Receptor Function and Location
| Receptor | Function | Location | Agonist | Antagonist |
|---|---|---|---|---|
| Alpha-1 (α1) | Constriction of smooth muscles |
|
|
|
| Alpha-2 (α2) | Inhibition of the sympathetic ganglia (i.e. - decreasing SNS activity) |
|
|
|
| Beta-1 (β1) | Increases cardiac performance, liberation of energy, and conservation of water |
|
|
|
| Beta-2 (β2) | Relaxation of smooth muscles (e.g. in the lungs), and liberation of energy |
|
|
|
Modulating Sympathetic Activity
Most of the time, the SNS and PNS are opposing each other. Therefore, to change this balance, one system can be strengthened, or the other weakened.
Modulating Sympathetic Activity
| To increase (↑) sympathetic activity | To decrease (↓) sympathetic activity |
|---|---|
You want to increase stimulation of the α and β receptors:
| You want to decrease stimulation of the α and β receptors:
|
Parasympathetic Receptors
The following table details the function and location of parasympathetic receptors, as well as example agonists and antagonists.
Muscarinic (M) and Nicotinic (N)
Muscarinic (M) and Nicotinic (N) Receptor Function and Location
| Receptor | Function | Location | Agonist | Antagonist |
|---|---|---|---|---|
| Nicotinic (N) | “Nerve to nerve” and “nerve to muscle” communication |
|
|
|
| Muscarinic (M) | Opposes most sympathetic actions at the level of the organs |
|
|
|
How Does Succinylcholine Work?
Succinylcholine is a direct nicotinic receptor agonist but is used clinically as an indirect anticholinergic. It is a direct cholinergic agonist because it binds to the same binding site as acetylcholine and activates the receptor in the same manner. However, unlike endogenous acetylcholine, succinylcholine activates the nicotinic receptors so intensely that a depolarizing block occurs immediately followed by a desensitizing block (think of the phases of the action potential). This is what gives succinylcholine its paralyzing effects in anesthesia. In contrast, non-depolarising neuromuscular blocking agents (NMBAs), such as pancuronium, are direct cholinergic antagonists.Modulating Parasympathetic Activity
Most of the time, the SNS and PNS are opposing each other. Therefore, to change this balance, one system can be strengthened, or the other weakened.
Modulating Parasympathetic Activity
| To increase (↑) parasympathetic activity | To decrease (↓) parasympathetic activity |
|---|---|
You want to increase stimulation of the M (and N) receptors:
| You want to decrease stimulation of the M (and N) receptors:
|