- Last edited on June 7, 2023
Polysomnography (PSG)
Primer
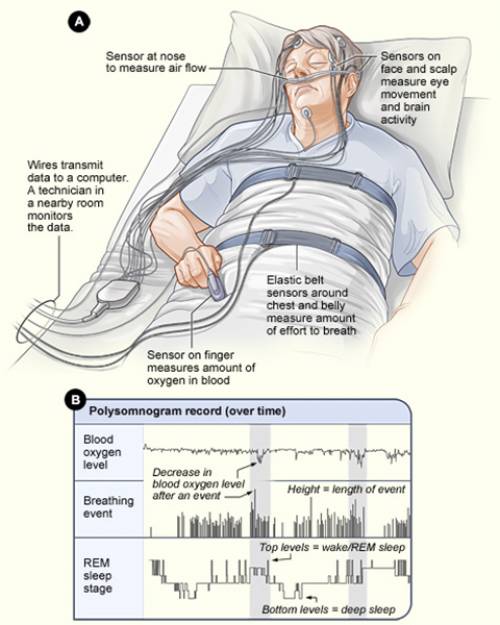
Polysomnography (PSG) is a multi-parametric test used in the study of sleep and as a diagnostic tool in sleep medicine.
Indications
- PSGs should be ordered if there is clinical suspicion for obstructive sleep apnea, parasomnias, periodic limb movements, narcolepsy, or REM sleep behaviour disorder.
- 3 to 4 hours of recordings is usually enough to detect the above conditions
When is a Polysomnogram Not Indicated?
PSGs are not routinely indicated for the evaluation of difficulty initiating or maintaining sleep (insomnia), circadian rhythm disorders, non-epileptic parasomnias, chronic lung disease, depression, bruxism, or behavior-based sleep disorders.Components
The components of a polysomnogram include the following:
- Electromyography (EMG), specifically the submentalis muscle (bruxism) and anterior tibialis (restless legs)
- Electro-occulogram (EOG), to monitor for rapid eye movements
- Electrocardiogram (ECG), to monitor cardiac function
- Oral and nasal airflow pressure and temperature (using nasal pressure transducer and thermistor)
- Chest and abdomen movement (i.e. - respiratory effort, measured using chest and abdominal belts)
- Oxygen saturation (using finger probe digital pulse oximetry)
- Transcutaneous CO2 (TcCO2)
During PSG, characteristic EEG, EMG, and EOG amplitudes and waveforms are scored in 30 second epochs.
Normal Sleep
Normal, non-pathological sleep is characterized by a sleep latency (from lights out to Stage 1 sleep) of <30 minutes and only brief arousals during sleep (<10 seconds). Any nighttime awakenings are also brief, cognitively and affectively neutral, and the individual is able to quickly return back to sleep. The recommended amount of sleep varies by age, but declines with age.[1] Ultimately, the required sleep time is individualized – it is the amount of sleep required for a person to feel rested and restored the next day. Normal sleep is also characterized by the absence of daytime sleepiness.
Recommended Sleep Time
Adapted from: Hirshkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation's sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1(1):40-43| Age Range | Recommended Hours of Sleep | |
|---|---|---|
| Newborn | 0-3 months old | 14-17 hours |
| Infant | 4-11 months old | 12-15 hours |
| Toddler | 1-2 years old | 11-14 hours |
| Preschool | 3-5 years old | 10-13 hours |
| School-age | 6-13 years old | 9-11 hours |
| Teen | 14-17 years old | 8-10 hours |
| Young Adult | 18-25 years old | 7-9 hours |
| Adult | 26-64 years old | 7-9 hours |
| Older Adult | 65 or more years old | 7-8 hours |
Rapid Eye Movement
Rapid Eye Movement (REM) sleep has two components: a parasympathetically-driven tonic component, and a sympathetically-driven phasic component. Phasic REM sleep is characterized by skeletal muscle twitches, increased heart rate variability, pupillary dilation, and increased respiratory rate. Tonic REM is characterized by EMG suppression (i.e. - no more muscle twitches), a high arousal threshold (much more difficult to wake up the individual), elevated brain temperature, poikilothermia (loss of thermoregulation), and penile tumescence (spontaneous erection).
All antidepressants (except for trazodone and bupropion) increase REM latency and suppress REM sleep. Atypical antipsychotic medications also generally suppress REM sleep, while increasing amounts of stage N3.
REM Latency
REM latency is the time from when someone falls asleep to the time of first onset of REM sleep. REM sleep occurs every 90 to 120 minutes throughout the night. Thus, changes in REM sleep latency are considered a markers for sleep-related disorders. Short/decreased REM latency (i.e. - a faster time to REM onset) can be due to:- First night of CPAP use
- Substance withdrawal (amphetamines, barbiturates, and alcohol)
- Major depressive disorder (more commonly in psychotic depression)
EEG
Sleep Stages
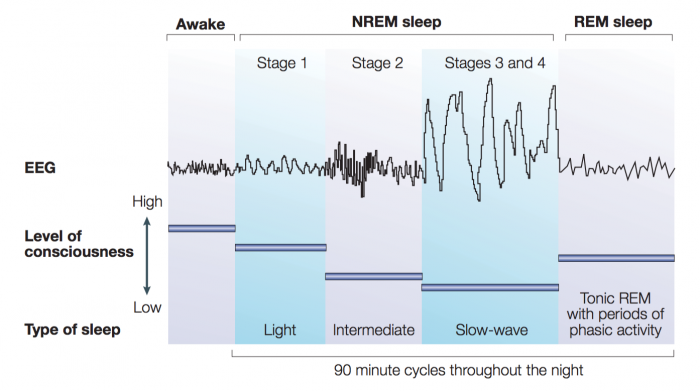
Sleep consists of two physiological states: non-rapid eye movement sleep (known as NREM) and rapid eye movement sleep (also known as REM):
- NREM sleep can be broken down into three stages: N1, N2, and N3 (or four stages based on: Stages 1, 2, 3/4).
- REM sleep is a different state of sleep characterized by high levels of brain activity and physiological activity similar to an awake state. REM sleep usually develops about 90 minutes after sleep begins. REM sleep on a polysomnograph appears the same as the awake stage. Therefore, REM cannot be identified by EEG alone, you need an EMG (and see absence of muscle activity) to confirm the presence of REM
Sleep Stages
| Stage of Sleep | % Total Sleep Time | Description | Function | EEG | Eye Movements | Muscle Tone |
|---|---|---|---|---|---|---|
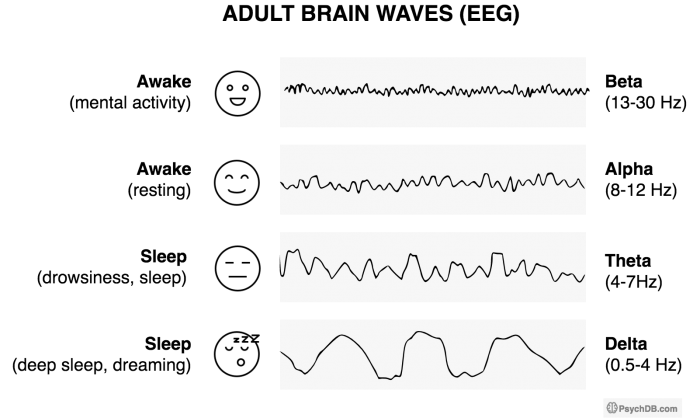
| Awake (eyes open) | - | • Alert and active mental focus | Wakefulness | • Beta, 15–60 Hz • This is the highest frequency, lowest amplitude EEG | Eyes move and blink | High voluntary tonic activity |
| Awake (eyes closed) | - | • Restful state but not sleeping | Wakefulness | Alpha waves, 8-12 Hz | Eyes move | High voluntary tonic activity |
| Stage N1 (Stage 1) | 5% | • Also known as “light sleep.” It is the transition from wakefulness → sleep and vice versa • Individuals may often be in this stage and think they are “not sleeping.” • Increased light quality sleep indicates sleep disruption | Prominent alpha waves = becoming more drowsy | • Theta waves (low amplitude, mixed frequency), 4-8 Hz and some alpha waves, 8-12 Hz • In N1, alpha makes <50% of EEG and is mixed with theta waves • Note that N1 can be very similar to a waking EEG | Slow rolling eye movements (SREMs) are usually the first evidence of drowsiness seen on the EEG | Decreasing levels of high tonic activity |
| Stage N2 (Stage 2) | 50% | • Most of the night is spent in N2! • Sleep spindles and K-complexes emerge during this stage and are thought to be the brain's way of evaluating potential threats (i.e. - external stimuli) while sleeping and to dampen arousals if the threats are not real. | • Sleep spindles (Sigma waves), 11-16 Hz • K-complexes (negative sharp wave followed by positive slow waves), 12-14 Hz | None | Low tonic activity | |
| Stage N3 (Stage 3 and 4) | 10-20% | • The “deepest” stage and hardest to awaken, also called Slow Wave Sleep (SWS) • Associated with sleep inertia when awoken in this stage • It is also the most restorative sleep. | This is homeostatic sleep (reduced BP, HR, cardiac output, RR). Growth hormone is released. | • Delta waves, 0.5-4 Hz • This is the lowest frequency, highest amplitude EEG | None | Low tonic activity |
| Rapid Eye Movement (REM) | 25% | • A “paradoxical state” that resembles awake state, except there is muscle • Arousal with increased oxygen use, increased variability of autonomic state (BP, HR). Increased brain temperature, cerebral glucose metabolism and cerebral blood flow. • Release of acetylcholine in the cortex is highest during wakefulness and also during REM sleep. • Occurs every 90 minutes, and REM length grows longer through the night. | Cognitive sleep, learning, cognitive restructuring. | • High (fast waves) and mixed frequency, with low voltage • Also includes: saw-tooth waves, theta activity, and slow alpha activity • Looks similar to EEG of awake individual with their eyes closed | Rapid eye movement | Almost total muscle paralysis (during tonic phase of REM). There can be very brief movement during phasic periods. |
Mnemonic
The mnemonicBAT-D (Think of a bat!) can be used to remember the order of brain waves from wakefulness → deep sleep. Also, using the Greek letters, you can correspond the symbols to the lower bounds Hz of each wave.B- Beta (β) [β looks like the numbers 1 and 3 mashed up – 13 Hz (lower bound)]A- Alpha (α) [α looks like half of an 8 – 8 Hz (lower bound)]T- Theta (Θ) [Θ looks partially like a 4 – 4 Hz (lower bound)]D- Delta (δ)
Mnemonic
The mnemonics below can be used to remember that:- Stage N
2is when bruxism (twoth grinding) occurs
REM Sleep
- REM sleep is also known as “paradoxical sleep” in that the EEG looks like the awake state (low voltage, mixed frequency). There is also sawtooth waves (4-8Hz) and rapid eye movements. During REM sleep, there is autonomic hyperarousal (increased blood pressure, tachycardia, and increased respiration rate), poikilothermic condition, penile erection, near total paralysis of skeletal muscles, and dreaming.
- REM occurs in a cyclical fashion, every 90 to 100 minutes
- The first episode of REM usually begins after 90 minutes of starting sleep
- The first episode of REM is short (<10 minutes), but subsequent episodes grow longer (15 to 45 minutes)
Sleep and PSG Changes
Sleep Across the Lifespan
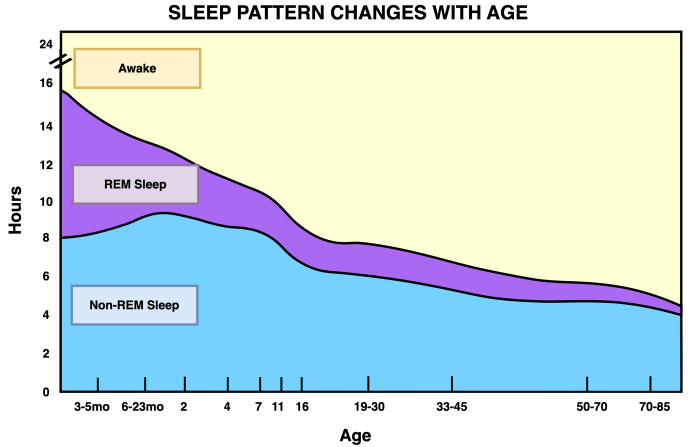
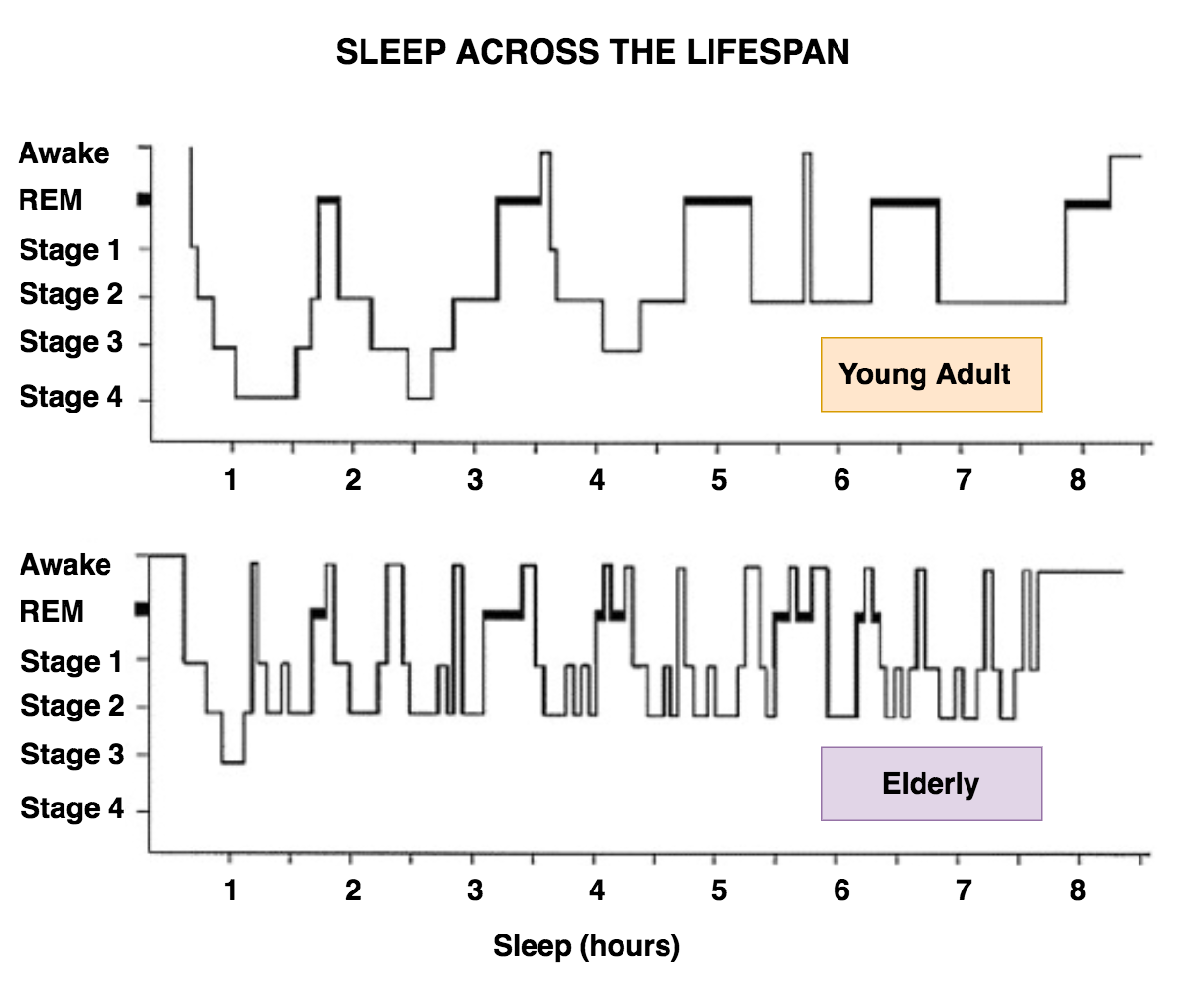
In early in life, about half of sleep time is spent in REM sleep. By adulthood, about 20% of sleep is REM sleep. REM sleep continues to decrease into old age. Older adults generally have more insomnia, find it harder to stay up late (due to relative advance of sleep phase), and have more shallow sleep. Sleep disruptions are common, including more brief awakenings. Sleep may also be less restorative, and there may be daytime sleepiness.
Older Adults
Insomnia is more prevalent in late life and sleep problems in the elderly are often mistakenly considered a normal part of aging. Sleep disturbance in older adults is associated with cognitive impairment, poor concentration, and decreased day-to-day functional performance. One of the challenges in identifying sleep disorders in older adults is that sleep architecture naturally changes significantly in healthy older adults (figure 5). In general with older adults:
- Initiation of sleep is harder
- Total sleep time (TST) and sleep efficiency are reduced
- Restorative sleep (i.e. - delta wave or slow wave sleep) decreases
- There is greater fragmentation of sleep, and there is generally longer time spent in bed awake
- The fragmentation begins at age 40
- REM sleep is usually preserved with age
- Sleep latency increases (harder to fall asleep faster).[4]
- Though some adults may be more somnolent, and this finding is not as well replicated
Medications
- Benzodiazepines, alcohol, and barbiturates can cause sleep spindles that can interfere with the quality of sleep
- REM sleep and Stage 3 sleep is reduced by benzodiazepines, alcohol, and barbiturates
- Monoamine oxidase inhibitors virtually completely remove REM sleep.[6]
Narcolepsy
In narcolepsy, changes in sleep include:
- Decreased REM latency (i.e. - REM sleep occurs almost immediately when someone sleeps)
Depression
Characteristic changes are seen in REM sleep in depression including:[7]
- Reduced REM sleep latency (individuals have earlier REM sleep)[8]
- Increased REM sleep density (there is greater concentration of REM sleep)[9]
- Decreased sleep efficiency (more time spent awake in bed)
- Decreased slow-wave sleep (meaning decreased N3, or stage 3 and stage 4 sleep)[10]
- More early morning awakenings (terminal insomnia), especially in major depressive disorder with melancholic features
- In general, antidepressants suppress REM sleep and increase REM latency, and thus antidepressants appear to normalize these changes in depression (except bupropion)