- Last edited on February 9, 2024
Obsessive-Compulsive Disorder (OCD)
Primer
Obsessive-Compulsive Disorder (OCD) is an obsessive-compulsive and related disorder that consists of (1) obsessions (intrusive, unwanted, and repetitive thoughts, urges, or images that don’t go away and are generally unwanted, or ego-dystonic) and/or (2) compulsions (repetitive physical behaviours or mental acts performed, meant to reduce the anxiety caused by the obsessions). Typical themes include contamination or cleaning, checking, symmetry, ordering or counting, as well as fears of harm to self or others. Obsessions can also be violent, sexual, or religious in nature.
Epidemiology
- There is a lifetime prevalence of 1 to 2% and it is highly disabling.
- OCD symptoms (not meeting the diagnostic threshold) are on a variant of normal; thus OCD symptoms occurs in over 25% of adults, and developmentally appropriate rituals and superstitions are common in children.
- The incidence of OCD has two peaks (a bimodal distribution), with different gender distributions: the first peak occurs between ages 7-12 (males>females), while the second peak occurs in early adulthood, around age 21 (females>males).[1]
- Although males typically present at an earlier age compared to females (25% of males in childhood), close to 60% of overall OCD diagnoses are female.[2]
Prognosis
- The initial onset of OCD is usually gradual, though acute onset is possible (but may warrant a more detailed neurologic work up). The course of OCD is typically chronic and fluctuating, although studies involving youth suggest that over half experience remission by early adulthood.
Comorbidity
- Anywhere between 60-90% of individuals with OCD also have a comorbid mental disorder, including mood, anxiety, somatoform disorders, substance use disorders, psychotic disorders, and bipolar disorders.
- In children, with OCD, there is a 5 to 7% incidence for Tourette's, and up to 30% have a life-time history of tics.[7]
- In children, OCD and ADHD are highly comorbid.[8]
- Lifetime prevalence for any co-morbid anxiety disorder (e.g. - panic disorder, social anxiety disorder, generalized anxiety disorder, specific phobia) is 76%.[9]
- Lifetime prevalence for any co-morbid mood disorder is 63%, with major depressive disorder being the most common (41%).[10]
- Comorbid obsessive-compulsive personality disorder (OCPD) is also common (between 23-32%).[11]
Risk Factors
- OCD has a strong neurobiologic basis and is highly heritable (half of all individuals have a family history of OCD; double the risk in those with a first degree relative and 10-fold risk if the relative's onset of OCD was in childhood or adolescence).[13]
- Environmental factors are also thought to play a role, including infectious etiologies and post-infectious autoimmune syndromes.
DSM-5 Diagnostic Criteria
Criterion A
Presence of obsessions, compulsions, or both:
Obsessions are defined by (1) and (2):
- Recurrent and persistent thoughts, urges, or images that are experienced, at some time during the disturbance, as intrusive and unwanted, and that in most individuals cause marked anxiety or distress
- The individual attempts to ignore or suppress such thoughts, urges, or images, or to neutralize them with some other thought or action (i.e. - by performing a compulsion)
Compulsions are defined by (1) and (2):
- Repetitive behaviors (e.g. - hand washing, ordering, checking) or mental acts (e.g. - praying, counting, repeating words silently) that the individual feels driven to perform in response to an obsession or according to rules that must be applied rigidly
- The behaviors or mental acts are aimed at preventing or reducing anxiety or distress, or preventing some dreaded event or situation; however, these behaviors or mental acts are not connected in a realistic way with what they are designed to neutralize or prevent, or are clearly excessive
Criterion B
The obsessions or compulsions are time-consuming (e.g. - take more than 1 hour per
day) or cause clinically significant distress or impairment in social, occupational, or
other important areas of functioning.
Criterion C
The obsessive-compulsive symptoms are not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication) or another medical condition.
Criterion D
The disturbance is not better explained by the symptoms of another mental disorder:
- excessive worries, as in generalized anxiety disorder
- preoccupation with appearance, as in body dysmorphic disorder
- difficulty discarding or parting with possessions, as in hoarding disorder
- hair pulling, as in trichotillomania
- skin picking, as in excoriation disorder
- stereotypies, as in stereotypic movement disorder
- ritualized eating behaviours, as in eating disorders
- preoccupation with substances or gambling, as in substance-related and addictive disorders
- preoccupation with having an illness, as in illness anxiety disorder
- sexual urges or fantasies, as in paraphilic disorders
- impulses, as in disruptive, impulse-control, and conduct disorders
- guilty ruminations, as in major depressive disorder
- thought insertion or delusional preoccupations, as in schizophrenia spectrum and other psychotic disorders
- or repetitive patterns of behaviours, as in autism spectrum disorder
Mnemonic
The mnemonic “Having OCD isMURDER” can be used to remember the criteria for obssessive-compulsive disorder.[14]
M- Mind (patient aware symptoms arise in the mind)U- Unpleasant thoughtsR- Resist (patient must want and try to resist the obsessive thoughts)D- Displeasure of feeling the obsessionE- Ego-dystonicR- Repetitive thoughts
Specifiers
Insight Specifier
- With good or fair insight: The individual recognizes that obsessive-compulsive disorder beliefs are definitely or probably not true, or that they may or may not be true.
- With poor insight: The individual thinks obsessive-compulsive disorder beliefs are probably true.
- With absent insight/delusional beliefs: The individual is completely convinced that obsessive-compulsive disorder beliefs are true.
Specifier
- Tic-related: The individual has a current or past history of a tic disorder.
Signs and Symptoms
- Many individuals with OCD have good or fair insight into their symptoms (able to understand their thoughts and beliefs are not rational), while some have poor insight. A small minority (around 4%) will have absent insight or delusion-like beliefs, which is linked to worse outcomes.[15]
- Obtaining a good history (see below) can elicit specific thoughts and behaviours that can guide towards a diagnosis of OCD.
Screening
Most individuals with OCD will have both obsessions and compulsions. High sensitivity screening questions and a good OCD history includes the following:
- Obsessions: Do you ever get intrusive or unwanted thoughts, images, or impulses that repeatedly enter your mind, despite you trying to get rid of them?
- e.g. - worries about dirt/germs, or thoughts of bad things happening
- Compulsions: Do you ever feel driven to do certain things over and over again?
- e.g. - repeatedly washing hands, cleaning, checking doors or work over and over, rearranging things to get it just right, or repeating thoughts in your mind to feel better?
- Does this waste significant time or cause problems in your life (Criterion B of DSM-5 criteria)?
- e.g. - interfering with school, work, or seeing friends?
The Relationship Between Obsessions and Compulsions
- Compulsions are usually performed in response to an obsession (e.g. - obsession about contamination → compulsion of hand washing rituals; obsession about a situation being incorrect → compulsion of repeating rituals until it feels “just right”)
- For individuals with OCD, compulsions reduce the distress triggered by the obsession, or prevent a feared event from occurring (e.g. - getting sick, hurting someone)
- It is important to note that compulsions are not connected in a realistic way to the feared event (e.g. - arranging items in a certain colour to prevent harm to a loved one) or are significantly excessive (e.g. - washing hands for 30 minutes at a time due to fears of contamination)
- Compulsions that are performed are not pleasurable! Rather, they allow the individual to experience relief from their anxiety or distress
History
Obsessions
Obsessions can be external or internal:
- External obsessions: contamination, objects, smells, asymmetry, mismatched items
- Internal obsessions: ego-dystonic thoughts (violent, sexual, etc.), always ask: “are these thoughts intrusive in nature?”
Common Obsessions
| Descriptions/Examples | |
|---|---|
| Contamination | Concerns about dirt, germs, body waste, illness |
| Symmetry | Needing things “just so”, even, or lined up a certain arbitrary way |
| Aggressive | Most commonly focused on inadvertent harm, such as being responsible for a fire or break-in; also includes horrific thoughts or images of deliberately harming others, such as stabbing a loved one or pushing a stranger in front of a car |
| Sexual | Disturbing sexual thoughts that are not consistent with an individual’s orientation or cultural norms, such as someone with a same-sex preference having unpleasant hetero-erotic thoughts, or unwanted inappropriate sexual thoughts about children |
| Religious | Examples include thoughts about selling one’s soul to the devil, deliberately thinking inappropriate thoughts about major religious figures, or committing mortal sins |
| Somatic | Exaggerated fears of contracting a serious illness such as hepatitis, or a brain tumour in the absence of any identifiable high risk |
Compulsions
Compulsions can be physical (behavioural) or mental (cognitive):
- Physical/behavioural compulsions: washing, checking, rearranging, reassurance seeking
- Mental/cognitive compulsions: mental rituals/review (“Did I actually do that obsession?”), replacing good thoughts with bad, counting, review
Common Compulsions
| Descriptions/Examples | |
|---|---|
| Washing | Excessive hand-washing, showering, or cleaning activities |
| Checking | Repeatedly turning the stove on and off; re-reading all emails to ensure content is appropriate; driving around the block to ensure didn’t hit someone; asking for repeated reassurance |
| Ordering | Folding clothes “just so”, or arranging all cans in the cupboard so the labels are facing out |
| Counting | Performing actions a certain arbitrary number of times, such as tapping each foot 4 times when getting out of bed |
| Repeating | Repeatedly going up and down the stairs or flushing the toilet; typically done to “cancel” out a bad thought or until it feels “right” |
What is the purpose of the compulsion in individuals with OCD?
- Prevention seeking: “I want to stop something bad from happening.”
- Reassurance seeking: “I need to know the bad thing didn't/will not happen.”
Rating Scales
Psychometric Scales for Obsessive-Compulsive Disorder
| Name | Rater | Description | Download |
|---|---|---|---|
| Yale–Brown Obsessive Compulsive Scale (Y-BOCS) | Clinician/Self-report | A checklist and 10-item scale with severity rankings. It is the most widely used rating scale for OCD. Symptoms rated from 0 (none) to 4 (severe) in terms of: time spent, distress, resistance, control, and interference with functioning | |
| Florida Obsessive Compulsive Inventory (FOCI) | Patient | A self-rated measure also used in monitoring OCD symptoms |
Pathophysiology
Functional neuroimaging from PET, fMRI, and SPECT have shown that several brain structures are implicated in OCD:
- Caudate nucleus (located in the basal ganglia), is responsible for learning and memory (feedback), action selection, and integration with emotional information. Imaging studies have shown increased levels of activity during active symptoms, and activity levels normalize after successful treatment with medications or cognitive behaviour therapy.[16]
- Both CT and MRI studies have found smaller caudate size in individuals with OCD as well
- Orbitofrontal cortex, area responsible for decision-making, planning behaviours, reversal learning (i.e. - inhibiting old responses)
- Thalamus, the brain's “switchboard”, which is “hard-wired” for primitive cleaning/checking behaviours.
- Anterior cingulate gyrus, area of the brain responsible for error detection
Substance/Medication-induced Symptoms
- There is some emerging evidence that second-generation antipsychotics, in particular clozapine and olanzapine, can cause de novo obsessive compulsive symptoms (not disorder) or exacerbate pre-existing symptoms.[19][20] Stimulant medications for ADHD may also exacerbate OCS or cause de novo symptoms.[21]
PANDAS
Differential Diagnosis
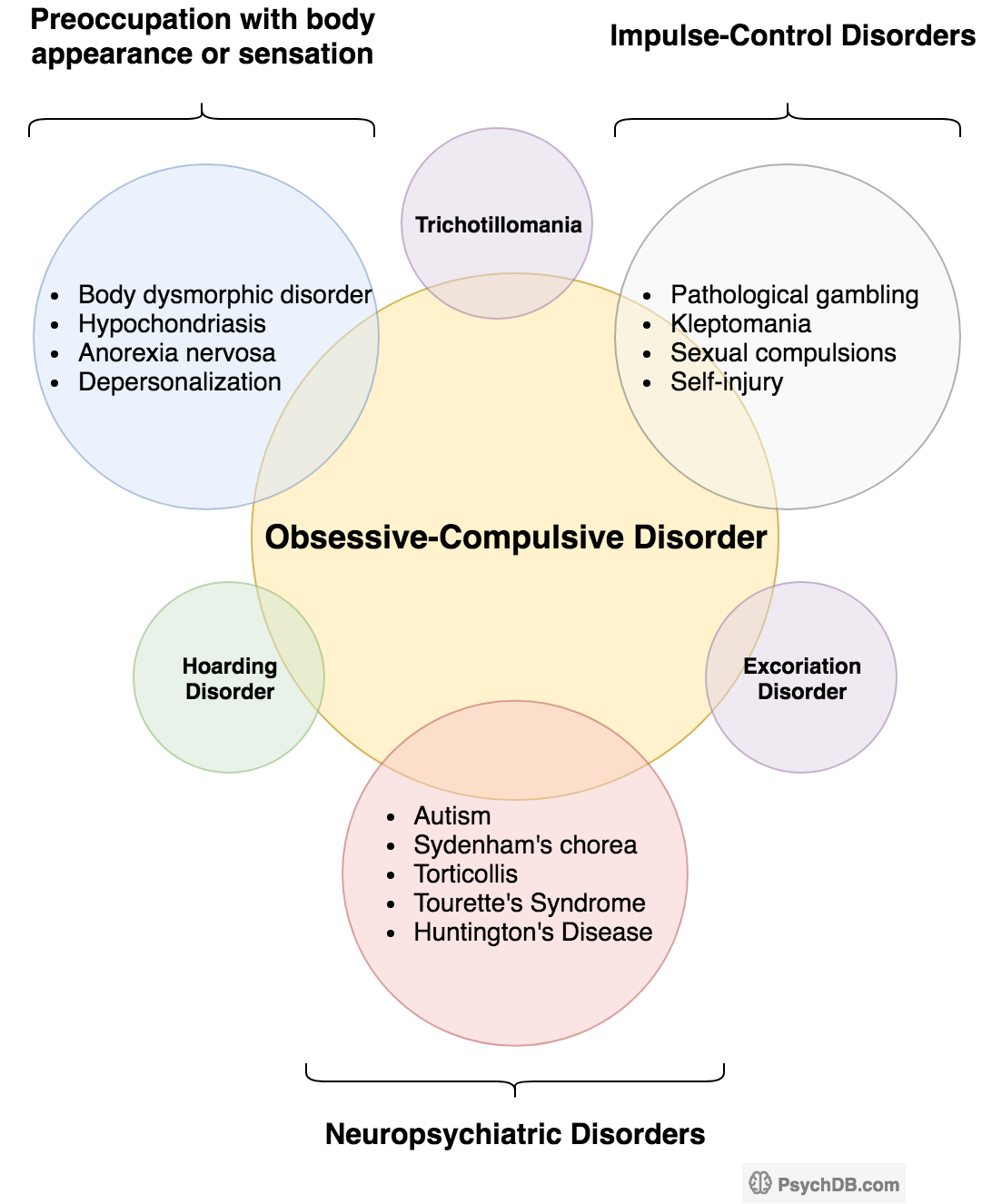
The differential diagnosis for OCD includes anxiety disorders, depression, complex tics, eating disorders, and psychosis. OCD is considered to be on a spectrum that encompasses comorbid conditions like hoarding disorder, excoriation disorder, trichotillomania disorder and body dysmorphic disorder. All these conditions are generally characterized by specific types of preoccupations and/or repetitive behaviours. It is important that the clinician be aware of all of these related conditions, as they must be differentiated from one another. See also Criterion D of the DSM-5 diagnostic criterion.
- Substance/Medication-induced obsessive compulsive symptoms (OCS)
- Recent initiation of an atypical (second generation) antipsychotic that is temporally-linked to the symptoms.
-
- Avoidant behaviors, recurrent thoughts, and the need for reassurance is also common in anxiety disorders. However these are usually real-life concerns, compared to the obsessions in OCD which usually do not involve real-life concerns (which may be odd/irrational). In addition, there are usually both compulsions and obsessions.
-
- Similar to OCD, individuals with specific phobia may have a fear reaction to specific objects or situations. However, rituals are not present.
-
- In social anxiety disorder (social phobia), the feared objects or situations are limited to social interactions, and avoidance or reassurance seeking is focused on reducing this social fear.
-
- Rumination can occur in both OCD and depression. However rumination in depression is usually mood-congruent and not necessarily experienced as intrusive or distressing. Again, ruminations are not linked to compulsions, which is common in OCD.
-
- In body dysmorphic disorder, obsessions and compulsions are limited to concerns about physical appearance
- In BDD, checking behaviours (e.g. - looking in the mirror), will further increase distress, whereas in OCD, checking behaviours usually decrease distress
-
- In trichotillomania, the compulsive behaviour is limited to only hair pulling and there are no obsessions
-
- In hoarding disorder, the main symptoms are severe difficulty or distress in discarding one's possessions, and excessive accumulation of objects. However, if an individual has obsessions that are typical of OCD (e.g. - concerns about incompleteness or harm), and these obsessions lead to compulsive hoarding behaviors (e.g. - acquiring all objects in a set to attain a sense of feeling “just right” or not discarding books because they may contain information that could prevent harm), a diagnosis of OCD should be given instead.
- In hoarding, the individual usually holds a strong sentimental value and attachment towards the hoarded objects
-
- In OCD, the obsessions and compulsions go beyond concerns about weight, body image, and food.
-
- Some individuals with OCD will have very poor insight or even to the point delusional OCD beliefs. However, there will be obsessions and/or compulsions (thus ruling out delusional disorder) and an absence of other symptoms of schizophrenia or schizoaffective disorder such as hallucinations or thought disorder.
-
- Tics are sudden, rapid, recurrent, nonrhythmic motor movement or vocalization (e.g. - blinking, throat clearing). A stereotyped movement is a repetitive, seemingly driven, nonfunctional motor behaviour (e.g. - head banging, rocking, biting). Tics and stereotyped movements are typically less complex than compulsions and they are not performed to neutralize obsessions. However, differentiating between complex tics and compulsions can sometimes be difficult. One way to distinguish is that compulsions are usually preceded by obsessions, whereas premonitory urges often precede tics. Since there is high comorbidity between the two disorders, there are cases were both diagnoses may apply.
-
- Obsessive-compulsive personality disorder (OCPD) and OCD have similar sounding names, but are two distinct entities. There are no intrusive thoughts, images, urges or repetitive behaviors in OCPD. Individuals instead have long-standing, pervasive maladaptive patterns of excessive perfectionism and rigid control. However, it is possible to have both diagnoses.
Is it anxiety, psychosis, or OCD?
One of the key features of OCD is that the obsessions/compulsions are egodystonic, meaning the individual does not want these thoughts (it's distressing!). In generalized anxiety, the worries are usually egosyntonic, meaning the individual feels the worries are beneficial to some degree. Similarly, psychosis (specifically delusions) can be confused with OCD. Again, individuals with OCD usually have insight that their symptoms are causing an impairment. Individuals with delusions/psychosis usually lack insight. However, in clinical practice, it can sometimes be difficult to distinguish between the three.[24] This is where clinical experience and good history taking comes in! Note also that children generally do not have good insight into their symptoms.[25]Is it somatic delusions/illness anxiety disorder or OCD?
- Individuals with somatic delusions or illness anxiety disorder are convinced that that they have an illness (e.g. - AIDS), despite testing results or medical reassurance.
- The worries in illness anxiety focus solely on health and disease
- The worries are always secondary to a misinterpretation of bodily symptoms, not an intrusive thought
- On the contrary, individuals with OCD are preoccupied that they could be infected or are performing excessive rituals to prevent this.
Investigations
- Anti-streptolysin O (ASO) and anti-DNAse B titres should be ordered if there is an acute or dramatic onset, or exacerbation of symptoms
Physical Exam
- As clinically indicated.
Treatment
- Various treatment guidelines exist for the treatment of OCD (see below for list of guidelines). The following treatment recommendations are based on the 2014 Canadian Clinical Practice Guidelines for anxiety, posttraumatic stress and obsessive-compulsive disorders:[26]
Education is Key!
- OCD is a chronic mental disorder that can be difficult to treat.
- Thus, whether you are treating with medications or psychotherapy, is it important to set realistic expectations as well as goals of treatment.
- Review the nature of the illness with your patient – that OCD is a chronic illness.
- Normalize the symptoms that your patients are experiencing.
- Realistic expectations include acknowledging that the OCD may not be cured, but that the goal is to improve function and reduce impairment.
- Those on medications need to understand that there is a lag time between medication initiation and response (up to 3 months).
- Those doing therapy need to understand there is an extensive time commitment involved as well.
Medications or CBT?
- CBT is very effective, safer, and more long-acting than medications.
- However, it does require motivation and hard work. It may be difficult to do CBT is an individual has comorbidities or is dealing with other major stressors.
- CBT may also be difficult to access in certain areas.
- Medications are “easy” to take and does help in OCD, but its benefits are limited compared to CBT.
- Additionally, there are side effects of medication to consider.
- Finally, the effects of medications are less enduring, and the risk of relapse is greater.
- See also: OCD Treatment Algorithm
Psychotherapy (ERP)
A specialized form of CBT, called Exposure and Response/Ritual Prevention Therapy (ERP) is the gold standard and first-line treatment for OCD, and favoured over medications.
- In ERP, patients are exposed to situations that trigger obsessions, and are taught strategies to prevent the compulsive response that would temporarily relieve their anxiety.
- Patients gradually become desensitized to the feared stimulus, resulting in improved OCD symptoms.
- The “Exposure” in ERP refers to exposing the patient to the thoughts, images, objects and situations that make them anxious and/or trigger the obsessions.
- The “Response Prevention” part of ERP, involves teaching the patient to not perform those compulsive behaviors once those anxiety or obsessions have been triggered; instead, they are taught to perform an opposite action.
- To do ERP successfully, patients must have significant buy-in into the therapy, as it can be a very distressing experience.
- Long-term maintenance of improvement has been shown in both children and adults.
- An sample structure of ERP would include:
- Delineating the range of obsessional triggers
- Establishing the range of discomfort associated with each trigger
- Establishing a hierarchy and rating the distress of each item (see example)
- Treatment then proceeds by systematically exposing the patient to each of the triggers with prevention of rituals
- There is a concurrent active homework schedule (e.g., 4 exposures per week, 2 hours each)
PsychDB is an Amazon Associate and earns from qualifying purchases. Thank you for supporting our site!
Sample Exposure Hierarchy for OCD
| Distressing Situation/Item | Distress (Scale 0 to 100) |
|---|---|
| Most distressing: touching public washroom door handle | 100 |
| 2nd most distressing: pumping gas | 70 |
| 3rd most distressing: gardening with gloves; turning stove on/off | 50 |
| 4th most distressing: washing off cans, bottles, bags | 40 |
Exercise
- The improvement in symptoms are hypothesized to be due to increased levels of brain-derived neurotrophic factor (BDNF), improved cerebral blood flow, increased volume to the hippocampus, enhanced cognitive and neuropsychological functioning, and improved resilience and overall well-being.
Medications
- Treatment with medications should be considered if CBT with ERP does not improve OCD symptoms sufficiently or is not feasible (i.e. - patient cannot face their symptoms directly).
- Well-designed studies have shown that there is no difference between ERP alone versus ERP plus pharmacotherapy. Remember that treating with medications alone confer only a marginal improvement in symptoms (CBT is important!)!
- It is important to set up a patient's expectations of how much improvement they will have on medications (patients can expect a maximum of a 30-35% reduction a medication).
- Remember too that relapse is also more likely with discontinuation of SSRI therapy compared to CBT/ERP.
- Patients must also be treated longer (at least 3 months) with doses near the maximum recommended doses (resulting in increased rates of adverse effects).[32]
- Intravenous clomipramine has also been shown to be as effective, and if not more effective than SSRIs.[33]
- It is important to monitor for serotonin syndrome if the patient is on both an SSRI and clomipramine.
- There is overall a low placebo response rate to medications (compare this to major depressive disorder, where the placebo response can be at least 35%).[34]
General Pharmacotherapy Principles for OCD
- Treatment is long-term (>1 year is recommended)
- Dosage reduction can be considered 3-6 months after that
- If 1st line treatment is unsuccessful, at least 2 other medications (SSRI, SNRI, or clomipramine) should be tried. Augmentation with a second medication is also another option
- Medications can be started at the usual dose and increased q5-7 days
- Highest doses work the best, and it may take 6-8 weeks to see the improvements
- An “adequate trial” for one medication is between 12-15 weeks, with at least 6 weeks at the maximum dose
- Symptoms should always be monitored via a scale like Y-BOCS
- When tapering or stopping medications, the taper should be done very slowly. There are high relapse rates unless the taper is combined with behavioural strategies or CBT!
- The focus of treatment should be for improvement in symptoms, and not complete remission
Pharmacotherapy for OCD
Katzman, M. A. et al. (2014). Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress and obsessive-compulsive disorders. BMC psychiatry, 14(S1), S1.| 1st line | Monotherapy: escitalopram, fluoxetine, fluvoxamine, paroxetine, sertraline |
|---|---|
| 2nd line | Monotherapy: citalopram, clomipramine, mirtazapine, venlafaxine XR |
| 3rd line | Monotherapy: IV citalopram, IV clomipramine, duloxetine, phenelzine, tramadol, tranylcypromine |
| Adjunctive therapy | First-line: aripiprazole, risperidone Second-line: memantine, quetiapine, topiramate Third-line: amisulpride, celecoxib, citalopram, granisetron, haloperidol, IV ketamine, mirtazapine, N-acetylcysteine, olanzapine, ondansetron, pindolol, pregabalin, riluzole, ziprasidone Not recommended: buspirone, clonazepam, lithium, morphine |
| Not recommended | Clonazepam, clonidine, desipramine |
Medication Dosing for OCD
Note that dosing of medications for OCD typically requires higher doses than that used for other psychiatric disorders.| Medication | Dose |
|---|---|
| Clomipramine | 150-250mg PO daily[35] |
| Fluoxetine | 20-80mg PO daily |
| Fluvoxamine | 150-300mg PO daily |
| Sertraline | 100-200mg PO daily |
| Paroxetine | 20-80mg PO daily |
| Escitalopram | 10-50mg PO daily* |
| Citalopram | 20-80mg PO daily* |
If First-line Drugs Aren't Working...
- Switch: try at least 2 different SSRIs
- Augment: with an antipsychotic
- Consider other 2nd line agents
- Other (off-label) augmentation strategies include:
- Glutamate modulating agents: topiramate, riluzole, memantine
- Mood stabilizers: lithium, valproate, gabapentin (to enhance serotonergic neurotransmission)
Residential
Children
- For children and adolescents, psychological treatments are generally preferred over pharmacotherapy.
- If medications must be used, fluoxetine is the most commonly used medication.[38]
- However, sertraline and fluvoxamine have also been found to be effective. In OCD, the addition of CBT in those with partial response to SSRIs is superior to SSRIs alone.[39]
Refractory OCD
- Treatment-refractory OCD is defined as failing to achieve adequate symptom relief despite receiving an adequate course of CBT and at least 2 adequate trials of selective serotonin reuptake inhibitors (SSRI) (or clomipramine).
- When refractory, pharmacotherapy and outpatient CBT are often ineffective. In some cases, individuals may opt for residential treatment with more intensive therapy.
- Other biological therapies under investigation include Repetitive Transcranial Magnetic Stimulation (rTMS), deep brain stimulation, and psychosurgery.
- Capsulotomy and cingulotomy have been effective in reducing symptoms in severe cases, but remain experimental last-resort treatments.[40]
Guidelines
OCD Guidelines
| Guideline | Location | Year | Website | |
|---|---|---|---|---|
| Canadian Clinical Practice Guidelines | Canada | 2014 | - | Link |
| National Institute for Health and Care Excellence (NICE) | UK | 2005 | - | Link |
| American Psychiatric Association (APA) | USA | 2007, 2013 | - | • Guideline (2007) • Guideline Watch (2013) • Quick Reference |