- Last edited on July 18, 2024
Dialectical Behavioural Therapy (DBT)
Primer
Dialectical Behaviour Therapy (DBT) is a psychotherapy developed by Marsha Linehan in the 1980s to treat borderline personality disorder. Many of the principles of DBT are rooted in mindfulness. DBT can also be used broadly in the treatment of depression, self-harm, suicidal ideation/attempts, and anxiety.
Indications
Although DBT is primarily used for treatment of borderline personality disorder, there is also evidence for its use in depression, substance use disorders, posttraumatic stress disorder, traumatic brain injuries, and binge-eating disorder.[1]
How Does It Work?
What Does Dialectical Even Mean?
DBT is based on the idea that life is full of opposites, and that these contradictions can cause distress. DBT helps patients learn that two opposing things can still be true at the same time (by using the term 'and' instead of 'but'). Additionally, DBT encourages patients to accept these apparent opposites through acceptance and change. By embracing contradictory ideas in life and changing them into dialectical statements, it allows us to move away from extremes in thinking and behaviour. Marsha Linehan specifically defines the term 'dialectical' as the “synthesis or integration of opposites”.[2] Examples of dialectical ideas in DBT include:- An emotion can be valid and not helpful at the same time
- I can strongly believe in a thought and that thought may not be true
- You can love someone and be angry at them at the same time
- Experiencing life can lead to pain and despair and experiencing life can lead to joy and meaning
Efficacy
- The response rate to DBT is approximately 75%, with a drop out rate between 30-40%.[3]
- There is strong evidence that shows DBT (specifically the group skills training component) reduces self-harm and suicide attempts in highly suicidal self-harming adolescents.[4]
- There is also robust evidence for the use of DBT in individuals with bipolar spectrum disorders and reducing suicidal behaviours.[5]
- The implementation of broad-based, universal DBT (specifically the group skills training component) in school curricula has not been shown to reduce depressive and anxiety symptoms, and paradoxically, the intervention arm in a 2023 study showed poorer parent-child relational quality.[6]
- Similarly, another trial showed that brief online dialectical behavior therapy skills training paradoxically increased the risk for self-harm behaviours, compared to controls.[7]
Length
- DBT is a time-limited therapy. It remains unclear what an adequate treatment length for DBT is (i.e. - 6 months vs. 1 year), and the research evidence is unclear.[8]
Structure
A detailed assessment is required before starting a course of DBT. Progress with therapy is tracked at weeks 1, 3, and 5. Patients are augmented with medications as needed. If the patient is not adhering to therapy, then they are recommended to consider stepping up to in-person group or individual therapy.
Stages
There are 4 stages of DBT (details of which will not be explained here). In brief, the first stage (Stage I) focuses on reducing of out-of-control behaviours that fall into 3 categories and are ranked in terms of importance as follows:
- Life-threatening behaviours
- (e.g. - suicide, self-harm, severe aggression, severe anorexia and not eating, over-eating in the morbidly obese, alcohol use with liver cirrhosis, anything that places one at imminent risk)
- Therapy-interfering behaviours
- (e.g. - showing up late for DBT appointments or not showing up at all, or behaviours that interfere with therapist’s motivation to treat client)
- Severe quality-of-life-interfering behaviours
- (e.g. - substance use, impulsive spending, less prominent eating disorders, inability to keep employment, educational problems, angry outbursts)
Once a patient has achieved reasonable control of severely dysfunctional actions, they can move to the next stage of treatment. Therapy in Stage II shifts its focus to increase a client’s ability to experience emotions without also experiencing trauma.[9] In Stage III, the goal is to synthesize the skills and insights gained to decrease symptoms that interfere with the achievement of personal goals. In the final stage, Stage IV, therapy focuses on resolving the client’s residual feelings of incompleteness, which may remain after the first 3 stages of therapy.
Components
The four main components of DBT are:
- Group skills and therapy
- One-on-one therapy
- 24 hour availability and access of the clinician to the patient, or session coaching
- Therapist meetings (where therapists consult each other and provide support)
Therapist Techniques
Behavioural Chain Analysis
Behavioural Chain Analysis (also known as functional analysis) is another technique used in DBT to help an individual understand the function of a particular behaviours. During a chain analysis of a problem behaviour (e.g. - cutting and self-harm), the individual tries to uncover all the factors that led up to that behaviour. In the analysis, the therapist works with the patient to identify vulnerabilities, triggers for the behaviours, and links in the chain that lead to the final behaviour.
Validation
Validation is a core component of DBT. Marsha Linehan developed the Six Levels of Validation for use in DBT (see this great article for more information):
- Being present
- Accurate reflection
- Reading a person's behaviour and guessing what they might be feeling
- Understanding the person’s behaviour in terms of their history and biology
- Normalizing or recognizing emotional reactions that anyone would have
- Radical genuineness
DBT Skills
Learning and practising interpersonal effectiveness skills are a core component of DBT. Thinking about a patient's presentation in the context of the Stress-Vulnerability Model can help patients choose to use which skills at what time. There are four key skills that should be learned in therapy:
- Emotion regulation
- Interpersonal effectiveness
- Distress tolerance
- Mindfulness
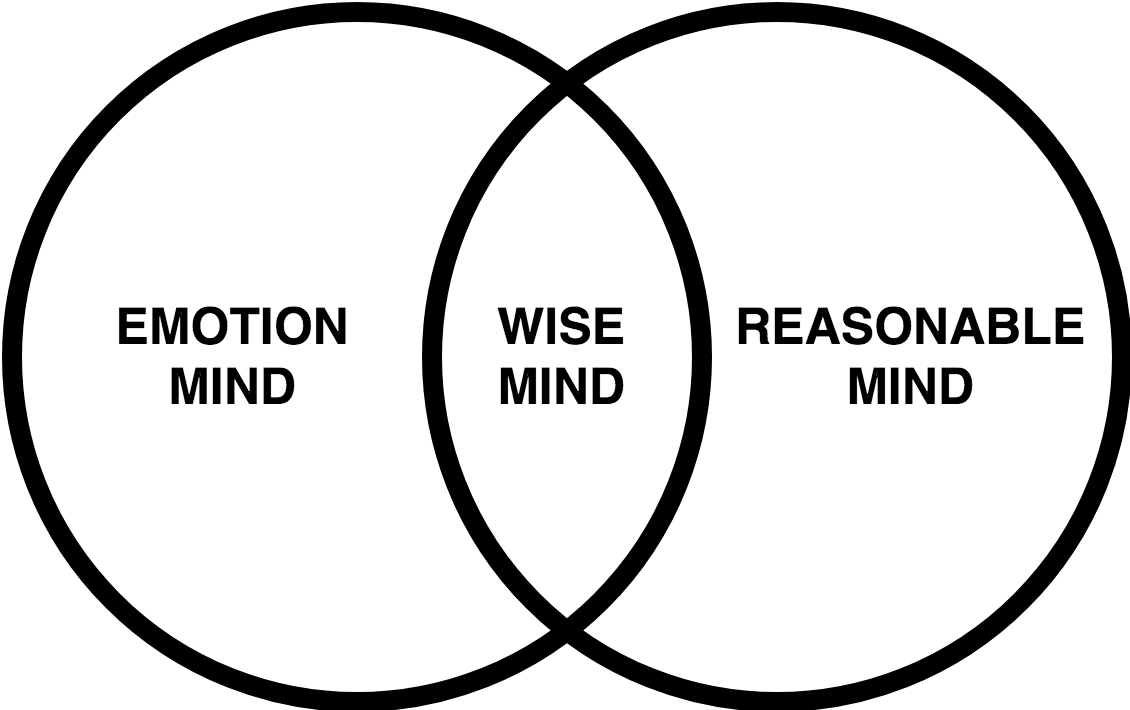
Wise, Emotion, and Rational Mind
- Emotion Mind is hot, mood-dependent, and emotion-focused. When in emotion mind, you are ruled by your moods, feelings, and urges to do or say things. Facts, reason, and logic are not important. Sometimes we also just need to accept and come to terms that we are in emotion mind.
- Reasonable Mind is cool, rational, and task-focused. When in reasonable mind, you are ruled by facts, reason, logic, and pragmatics. Values and feelings are not important. The benefit of being in reasonable mind is you do not have to name of experience feelings.
- Wise Mind is the inner wisdom that each one of us has. When we access our inner wisdom, we say we are in Wise Mind. When we enter the state of Wise Mind, we integrate opposites (both the reasonable and emotional mind) and are open to experiencing reality as it is. Wise Mind is the middle path between two extremes. In Wise Mind, we replace “either-or” thinking with “both–and” thinking to find synthesis between oppositions. Remember, when we are at an extreme on any continuum, we are in danger of distorting reality. It is also important to acknowledge that you do not have to be perfect even when you are in wise mind.
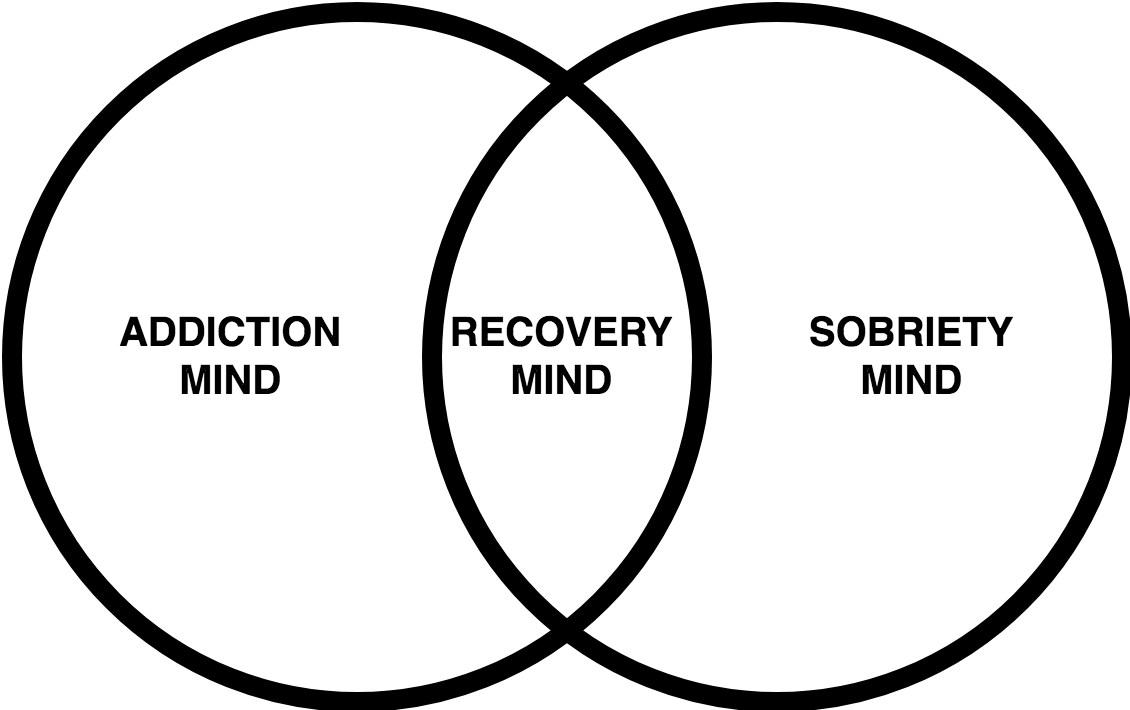
Recovery, Addiction, and Sobriety Mind
The principles of Wise Mind, Emotion Mind, and Reasonable Mind can also be applied towards addictions.
- Addiction Mind is a mind that completely 'gives up' on oneself to the negative aspects of addiction
- Sobriety Mind is a mind that thinks one is not at all vulnerable to addiction
- Recovery Mind is aware of both the negative and powerful aspects of addiction
Mindfulness
"What” Skills
“What” Skills are what you do when you practice mindfulness: observe, describe, or participate. Do only one of these activities at a time.
- Observe - pay attention on purpose to the present moment
- Describe - put into words what you have observed
- Participate - enter into an activity fully and wholly, becoming one with whatever you are doing
"How" Skills
“How” Skills are how you practice when you practice mindfulness: nonjudgmentally, one-mindfully, and effectively. Although the “what” skills should only be done one at a time, the “how” skills can be done together.
- Nonjudgmentally
- One-mindfully
- Effectively
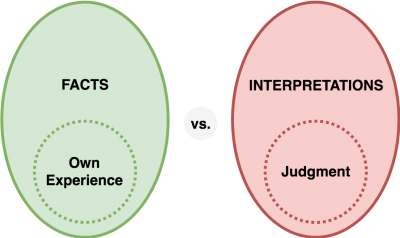
Check the Facts
Check the Facts is a core strategy in also used in other cognitive therapy interventions like cognitive behavioural therapy. Humans often react to our thoughts and interpretations of an event rather than to the facts of the event. Checking the facts means checking if our emotional reactions actually fit the facts of the situation. It also means looking out for interpretations, judgments, and opinions. Avoid “good vs. bad”, “should vs. shouldn't” and other judgmental language. Instead try to use language like “this is helpful or not helpful.” Changing our beliefs, assumptions, and interpretations of events to fit the facts can change our emotional reactions.
Opposite Action
Use opposite action when your emotion or its intensity does not fit the facts.
Emotions and Opposite Action
Adapted from Skills Training Manual for Dialectical Behavior Therapy Marsha Linehan © 2014 Guilford| Emotion | |
|---|---|
| Love | • AVOID the person, animal or object you love • DISTRACT from thoughts of the person animal or object • REMIND yourself of the “cons” of loving • Do the OPPOSITE of other loving action urges |
| Sadness | • Get ACTIVE; approach, do not avoid. • Do things that make you FEEL COMPETENT and self-confident. |
| Shame | When your behaviour does not violate your own moral values: • Make your personal issues PUBLIC with people who won’t reject you • Engage in behavior that sets off shame OVER AND OVER in public • Do the OPPOSITE of other shame action urges When your behaviour does violate your own moral values: • APOLOGIZE publically • REPAIR the transgression • MAKE THINGS BETTER; or work to prevent or repair similar harm for others • COMMIT to avoiding that mistake in the future • ACCEPT the consequences gracefully |
| Guilt | When you will not be rejected if found out: • Make your personal characteristics PUBLIC with people who won't reject you • Engage in behaviour that sets off guilt OVER AND OVER AND OVER in public When you will be rejected if found out: • HIDE or USE SKILLFUL MEANS if you want to stay in the group • Join a NEW GROUP that fits your values • Do what makes you feel guilty OVER AND OVER with your new group |
Emotions and Opposite Action
Adapted from Skills Training Manual for Dialectical Behavior Therapy Marsha Linehan © 2014 Guilford| Emotion | Opposite Action |
|---|---|
| Fear | • Do what you are afraid of doing over and over again • APPROACH events, places, tasks, activities, people you are afraid of • Do things to give yourself a sense of CONTROL and MASTERY over your fears |
| Anger | • Gently AVOID person you are angry with (rather than attacking) • Take a TIME-OUT and breath in and out deeply and slowly • Do something a little bit NICE (rather than mean or insulting • Do the OPPOSITE of other angry action urges |
| Disgust | • MOVE CLOSE. Eat, drink , stand near, or embrace what you found disgusting • Be KIND to those you feel contempt for; step into the other person's shoes |
| Envy | • Inhibit destroying what the other person has • Do the OPPOSITE of envious action urges • COUNT YOUR BLESSINGS • Make a list of the things you are thankful for |
| Jealousy | • LET GO of controlling others' actions • SHARE what and who you have in your life |
ABC PLEASE
Emotional distress and anguish can be reduced by decreasing risk factors that can make one more vulnerable to negative emotions and moods. The acronym ABC PLEASE can help with this.
ABC PLEASE
A- Accumulate positive emotions- Short-term: do pleasant things that are possible now
- Long-term: make changes in your life so that positive events will happen more often in the future. Build a “life worth living“.
B- Build mastery- Do things that make you feel competent and effective to combat helplessness and hopelessness
C- Cope ahead of time with emotional situations- Rehearse a plan ahead of time so that you are prepared to cope skillfully with emotional situations
P- (Treat) Physical illnessL- (Treat) PhysicaL illnessE- (Balance) EatingA- Avoid Mood-Altering SubstancesS- (Balance) SleepE- Exercise
DEAR MAN, FAST, GIVE
Interpersonal conflicts can arise when there is ineffective communication. DEAR MAN is a skill to ask for something effectively, say no to another’s request, or to resist pressure and maintain your point of view. GIVE is a skill aimed at maintaining or improving your relationship with the other person while you try to get what you want in the interaction. FAST is a skill to keep or improve your self-respect and self-esteem while you try to get what you want in an interaction. Think about what you want out of an interaction and pick a skill to use.
'DEAR MAN': 'Getting What I Want' is the Priority
D- Describe the situation (Describe just the facts, and only the facts)E- Express your feelings (Express how you feel)A- Assert yourself (One can be passive, aggressive, passive aggressive, or assertive. Choose to be assertive over the other methods of communication)R- Reinforce (By expressing thanks to the individual, or is there a benefit or 'something in it' for the other person?)M- Mindful (Focus on the task at hand, and don't let emotions or judgments come in the way)A- Appear confident (Notice the key word is 'appear')N- Negotiate (If you don't get what you want, it's important to negotiate)
Aggressive, Passive, Passive-Aggressive, and Assertive Approaches
| You | Others | |
|---|---|---|
| Aggressive | + | - |
| Passive | - | + |
| Passive-Aggressive | - | - |
| Assertive | + | + |
'GIVE': 'Keeping or Maintaining the Relationship' is the Priority
G- Gentle (Have a relaxed body language, if you body is relaxed, then your emotions are also relaxed)I- Interest (Show genuine curiosity, if is hard to be angry if you're curious. You can also show interest by nodding, having eye contact, and asking questions)V- Validate (Validation means showing the person that at least some part of their experience is legitimate, but only validate what makes sense to you)E- Easy Manner
'FAST': 'Self-Respect or Self-Esteem' is the Priority
F- (Be) Fair (Be fair to both your needs and the other person's needs)A- (No) Apologies (Don't say sorry unless you've hurt someone)S- Stick to Values OnlyT- (Be) Truthful
SMART Goals
When choosing goals, it is important to choose goals that follow the SMART acronym to ensure they can be feasibly done. A goal should feel 80% do-able and 20% challenging so as to strike the right balance.
S- SpecificM- MeasurableA- AchievableR- RealisticT- Time-Limited