- Last edited on June 7, 2023
Introduction to Sleep Medicine
Primer
Sleep is a naturally recurring state of mind and body, characterized by altered consciousness, relatively inhibited sensory activity, inhibition of nearly all voluntary muscles, and reduced interactions with surroundings. Adequate sleep is vital for good mental health, and there is a bidirectional relationship between neuropsychiatric disorders and sleep.[1]
Wakefulness
- Various neurotransmitters are involved in wakefulness and sleep:[2]
- Wake-promoting neurotransmitters include:
- Norepinephrine (adrenaline keeps people awake)
- Histamine (this is why anti-histamines make you sleepy)
- Histaminergic neurons have high levels of activity during wakefulness and vigilance, and have significantly decreased activity during NREM and REM sleep.
- Orexin (hypocretin) (a deficiency in this is a cause of narcolepsy)
- Dopamine
- Glutamate
- Sleep-promoting and wakefulness neurotransmitters include:
- Acetylcholine
- Acetylcholine plays the primary role in generating wakefulness and REM sleep
- Serotonin
- Serotonin is primarily involved in promoting wakefulness, but may also play a role in generation of REM sleep.[3]
- The posterior hypothalamus plays an important role in the regulation of sleep-wakefulness.
Physiologically Drowsy States
- Certain periods of the day also contribute to sleepiness and drowsiness. The afternoons (12pm to 1pm), and early evenings (4pm to 5pm) are physiologically drowsy states when people feel more sleepy.
- This is evidenced in certain cultures, like afternoon siestas in Spain.[4]
Physiology of Sleep
- The sleep cycle is regulated by the circadian rhythm, which is regulated by the suprachiasmatic nucleus (SCN) in the hypothalamus.
- The Circadian rhythm controls night-time release of adrenocorticotropic hormone (ACTH), prolactin (PRL), melatonin, and norepinephrine.
- The SCN is regulated by natural environment and natural light
- The SCN stimulates norepinephrine release, which targets the pineal gland, which then releases melatonin
Definitions
- Sleep latency (sleep onset latency) — the amount of time it takes you to go from being fully awake to sleeping
Prevalence of Sleep Disorders
The most common sleep disorders include:
- Insomnia (10-30%)
- Restless leg syndrome (2-15%)
- Parasomnias (5-10%)
- Obstructive sleep apnea (4-8%)
Comorbid Medical Conditions Increase Risk for Sleep Disorders
Individuals with medical conditions such as end-stage renal disease (ESRD) can have a much higher prevalence of sleep disorders including: sleep apnea, restless legs syndrome, and periodic limb movement disorder.[5] In ESRD, uremia is thought to be critical in the development of sleep disorders.Importance of Sleep
Health
- Sleep is also thought to play a role in amyloid clearance in the brain, and poor sleep may be linked to Alzheimer's Disease (AD).[8]
Children/Adolescents
- This past century has seen consistent and rapid drops in the sleep duration of children and adolescents. This is primarily due to lifestyle factors, and changes in technology use.
- Common categories of sleep disorders in children include insomnias, sleep-related breathing disorders, hypersomnias, circadian rhythm sleep disorders, and parasomnias.
Sleep History
The Sleep History is Critical!
Understanding how to take a good sleep history, sleep disorders, and treatments is critical. Sleep disturbance is a common feature in many (if not all) psychiatric disorders. Differentiating between normal sleep disturbances, a sleep disorder, or a sleep disturbance due to a psychiatric disorder is critical to getting the patient the right treatment.History of Presenting Illness
- Timeline of sleep complaint
-
- Snoring/apneic episodes
- Awaken gasping for breath
- Bruxism (teeth grinding)
- Awakening with a dry mouth[9]
- Morning headaches
-
- Pain which delays or prevents sleep
- Pain which awakens from sleep
Sleep Review of Systems
- Vivid or life-like visions as you fall asleep or wake up (hypnogogic/hypnopompic hallucinations)
- Sleep paralysis (inability to move as you are trying to go to sleep or when you wake up)
- Cataplexy (suddenly falling down when laughing at a joke or when surprised, or weakness or feel your body go limp when you are angry or excited)
- Acting out of dreams (e.g. - if you were dreaming of cycling, are you actually moving your feet?)
-
- Irresistible urge to move legs or arms
- Creeping or crawling sensation in legs before falling asleep
- Legs or arms jerking during sleep
- Parasomnias
- Do you ever talk in your sleep?
- Do you ever walk or do things (or eat, or in rare cases sexsomnia can occur) in your sleep?
- Nightmares
- Falling out of bed
Sleep Schedule
- Time in bed:
- Time to sleep onset:
- Number of nighttime awakenings and reasons (e.g. - nocturia, pain, etc.):
- Time of final awakening (any early awakenings):
- Total hours of sleep
- When you wake up do you feel rested? (i.e. - is sleep non-restorative; do you not feel rested when you wake up?)
- Daytime sleepiness (sitting/talking/driving/eating/standing)
- Napping (frequency and length)
- Safety: Falling asleep unintentionally in dangerous situations (e.g. - while driving)
- Situational sleeping patterns
- What time do you wake up when you're on vacation?
- What time do you wake up when you're working?
Sleep Environment
- Bedroom is (loud/quiet) and (light/dark)
- Mattress is (soft/hard)
- Sleeping with television on?
- Is sleep disturbed because of bed partner or children or pets?
Psychiatric Review of Systems
- Depression: mood, motivation, concentration, energy, appetite, psychomotor slowing
- Low mood
- Memory changes
- Poor concentration
- Irritability
- Anxiety: worries out of control, blanking out, fatigue, sleep change, keyed up, irritable, muscle tension
- Racing thoughts when trying to sleep
- Worry about whether or not they will be able to fall asleep
- Fatigue
- Anxiety during the day
Past Medical History
- GERD (reflux, heartburn, indigestion, and regurgitation, disrupting sleep)
- Nocturia/genitourinary
- Respiratory
- Wheezing or coughing disrupting sleep
- Sinus/nasal congestion or post-nasal drip disrupting sleep
- Shortness of breath disrupting sleep (COPD)
- Asthma/emphysema
- Hypertension
- Fibromyalgia
- Parkinson's disease
- Diabetes
- Anemia
- Stroke
- Seizures
- Traumatic brain injuries
Family History
- Sleep disorders
- Psychiatric/neurological disorders
- Dementia
Medications
- Over-the-counter sleep aids
- Prescription sleeping aids
- Other non-prescribed sleep aids
- Use of prescription medications unrelated to sleep
- Use of opioid medications (exacerbate sleep apnea!)
Substances
- Alcohol
- Caffeine (time of day: , amount: )
Social History
- Work history (night shifts, hours worked)
- Exercise (how often, what time of the day)
Physical Exam
- Height:
- Weight:
- BMI:
Scales
Measuring sleep quality can be done through scales, questionnaires, and sleep diaries:
Measurement Scales for Sleep Quality
| Name | Rater | Description | Download |
|---|---|---|---|
| Epworth Sleepiness Scale (ESS) | Patient | The ESS is a self-administered questionnaire with 8 questions. | ESS Information |
| Insomnia Severity Index (ISI) | Patient | The ISI has seven questions rated on a scale of 0 to 4.[10] | ISI Download |
| Pittsburgh Sleep Quality Index (PSQI) | Patient | The PSQI is an effective instrument used to measure the quality and patterns of sleep in adults. It differentiates “poor” from “good” sleep quality by measuring 7 components. | PSQI Download |
Investigations
Sleep can be measured objectively in one of several ways:
- Actigraphy (measure gross motor activity)
- Polysomnography (needs to be done in a clinic)
- Ambulatory portable monitoring device (“Level 3 Sleep Study“)
Sleep Stages
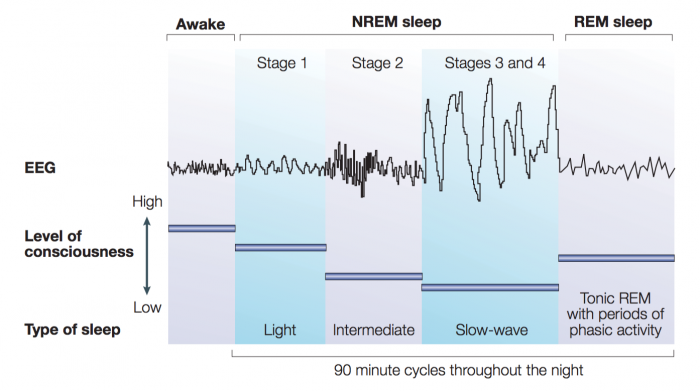
Sleep consists of two physiological states: non-rapid eye movement sleep (known as NREM) and rapid eye movement sleep (also known as REM):
- NREM sleep can be broken down into three stages: N1, N2, and N3 (or four stages based on: Stages 1, 2, 3/4).
- REM sleep is a different state of sleep characterized by high levels of brain activity and physiological activity similar to an awake state. REM sleep usually develops about 90 minutes after sleep begins. REM sleep on a polysomnograph appears the same as the awake stage. Therefore, REM cannot be identified by EEG alone, you need an EMG (and see absence of muscle activity) to confirm the presence of REM
Sleep Stages
| Stage of Sleep | % Total Sleep Time | Description | Function | EEG | Eye Movements | Muscle Tone |
|---|---|---|---|---|---|---|
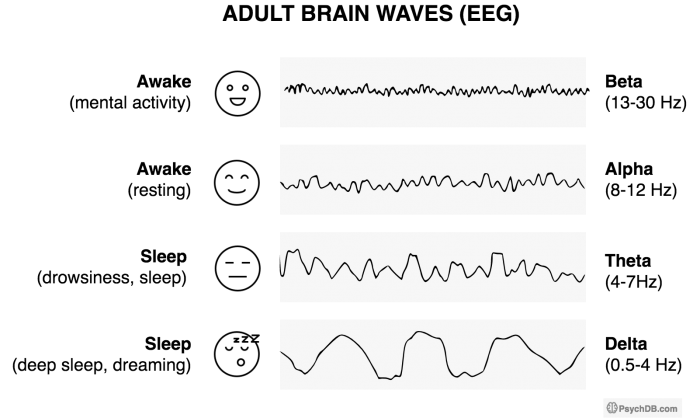
| Awake (eyes open) | - | • Alert and active mental focus | Wakefulness | • Beta, 15–60 Hz • This is the highest frequency, lowest amplitude EEG | Eyes move and blink | High voluntary tonic activity |
| Awake (eyes closed) | - | • Restful state but not sleeping | Wakefulness | Alpha waves, 8-12 Hz | Eyes move | High voluntary tonic activity |
| Stage N1 (Stage 1) | 5% | • Also known as “light sleep.” It is the transition from wakefulness → sleep and vice versa • Individuals may often be in this stage and think they are “not sleeping.” • Increased light quality sleep indicates sleep disruption | Prominent alpha waves = becoming more drowsy | • Theta waves (low amplitude, mixed frequency), 4-8 Hz and some alpha waves, 8-12 Hz • In N1, alpha makes <50% of EEG and is mixed with theta waves • Note that N1 can be very similar to a waking EEG | Slow rolling eye movements (SREMs) are usually the first evidence of drowsiness seen on the EEG | Decreasing levels of high tonic activity |
| Stage N2 (Stage 2) | 50% | • Most of the night is spent in N2! • Sleep spindles and K-complexes emerge during this stage and are thought to be the brain's way of evaluating potential threats (i.e. - external stimuli) while sleeping and to dampen arousals if the threats are not real. | • Sleep spindles (Sigma waves), 11-16 Hz • K-complexes (negative sharp wave followed by positive slow waves), 12-14 Hz | None | Low tonic activity | |
| Stage N3 (Stage 3 and 4) | 10-20% | • The “deepest” stage and hardest to awaken, also called Slow Wave Sleep (SWS) • Associated with sleep inertia when awoken in this stage • It is also the most restorative sleep. | This is homeostatic sleep (reduced BP, HR, cardiac output, RR). Growth hormone is released. | • Delta waves, 0.5-4 Hz • This is the lowest frequency, highest amplitude EEG | None | Low tonic activity |
| Rapid Eye Movement (REM) | 25% | • A “paradoxical state” that resembles awake state, except there is muscle • Arousal with increased oxygen use, increased variability of autonomic state (BP, HR). Increased brain temperature, cerebral glucose metabolism and cerebral blood flow. • Release of acetylcholine in the cortex is highest during wakefulness and also during REM sleep. • Occurs every 90 minutes, and REM length grows longer through the night. | Cognitive sleep, learning, cognitive restructuring. | • High (fast waves) and mixed frequency, with low voltage • Also includes: saw-tooth waves, theta activity, and slow alpha activity • Looks similar to EEG of awake individual with their eyes closed | Rapid eye movement | Almost total muscle paralysis (during tonic phase of REM). There can be very brief movement during phasic periods. |
Mnemonic
The mnemonicBAT-D (Think of a bat!) can be used to remember the order of brain waves from wakefulness → deep sleep. Also, using the Greek letters, you can correspond the symbols to the lower bounds Hz of each wave.B- Beta (β) [β looks like the numbers 1 and 3 mashed up – 13 Hz (lower bound)]A- Alpha (α) [α looks like half of an 8 – 8 Hz (lower bound)]T- Theta (Θ) [Θ looks partially like a 4 – 4 Hz (lower bound)]D- Delta (δ)
Mnemonic
The mnemonics below can be used to remember that:- Stage N
2is when bruxism (twoth grinding) occurs
Sleep and Polysomnography Changes
Sleep Across the Lifespan
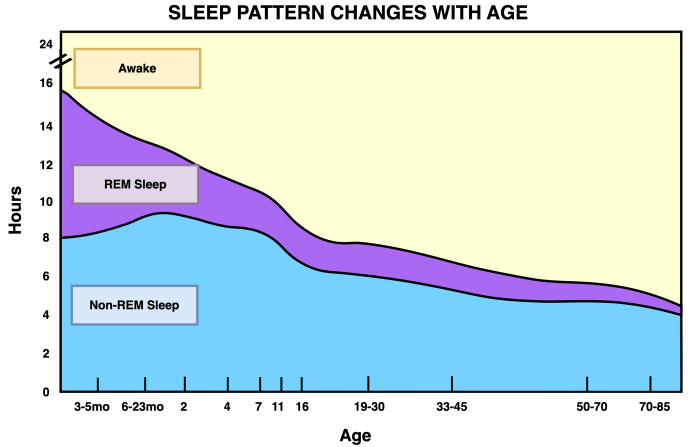
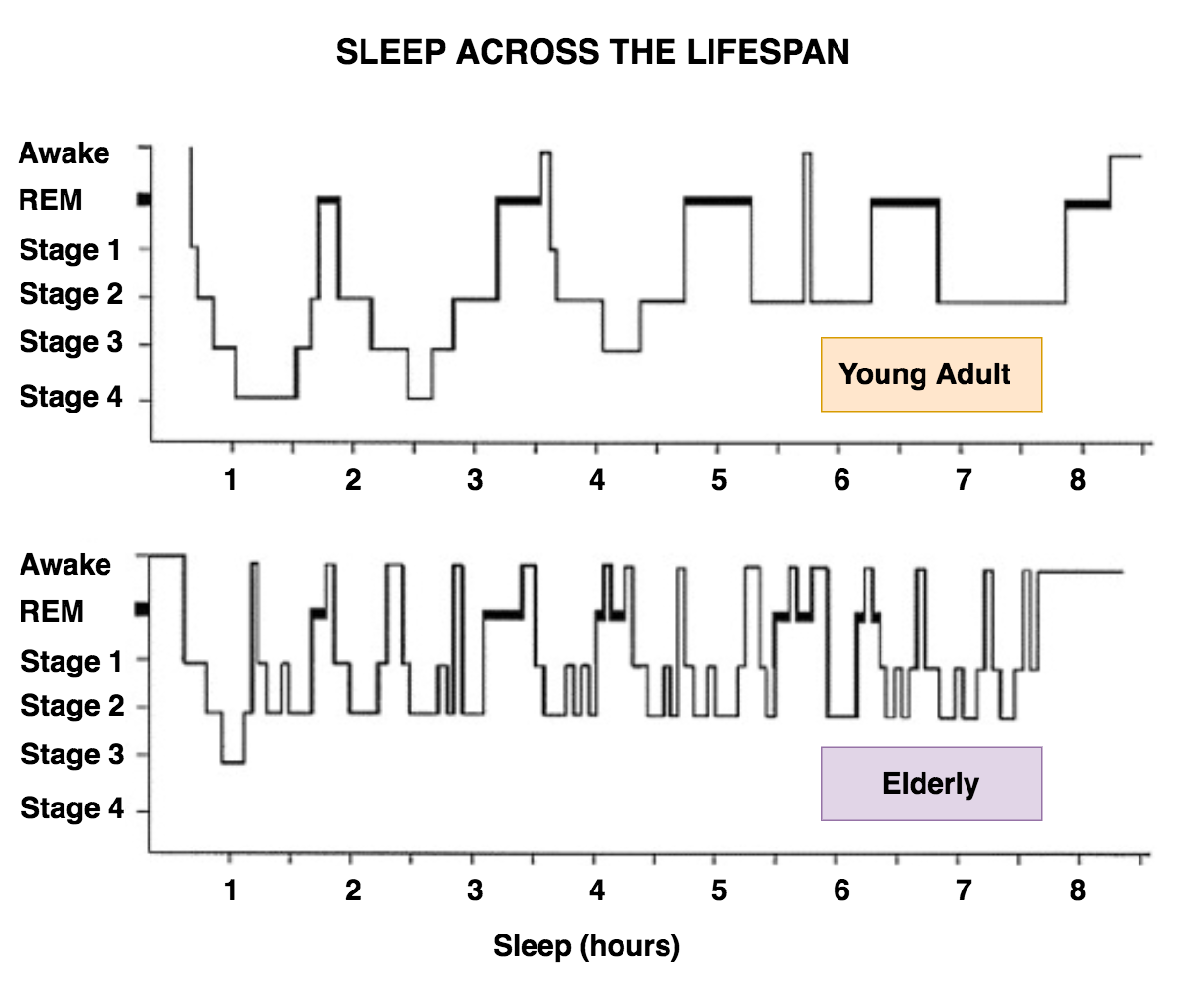
In early in life, about half of sleep time is spent in REM sleep. By adulthood, about 20% of sleep is REM sleep. REM sleep continues to decrease into old age. Older adults generally have more insomnia, find it harder to stay up late (due to relative advance of sleep phase), and have more shallow sleep. Sleep disruptions are common, including more brief awakenings. Sleep may also be less restorative, and there may be daytime sleepiness.
Older Adults
Insomnia is more prevalent in late life and sleep problems in the elderly are often mistakenly considered a normal part of aging. Sleep disturbance in older adults is associated with cognitive impairment, poor concentration, and decreased day-to-day functional performance. One of the challenges in identifying sleep disorders in older adults is that sleep architecture naturally changes significantly in healthy older adults (figure 4). In general with older adults:
- Initiation of sleep is harder
- Total sleep time (TST) and sleep efficiency are reduced
- Restorative sleep (i.e. - delta wave or slow wave sleep) decreases
- There is greater fragmentation of sleep, and there is generally longer time spent in bed awake
- The fragmentation begins at age 40
- REM sleep is usually preserved with age
- Sleep latency increases (harder to fall asleep faster).[13]
- Though some adults may be more somnolent, and this finding is not as well replicated
Medications
- Benzodiazepines, alcohol, and barbiturates can cause sleep spindles that can interfere with the quality of sleep
- REM sleep and Stage 3 sleep is reduced by benzodiazepines, alcohol, and barbiturates
- Monoamine oxidase inhibitors virtually completely remove REM sleep.[15]
Narcolepsy
In narcolepsy, changes in sleep include:
- Decreased REM latency (i.e. - REM sleep occurs almost immediately when someone sleeps)
Depression
Characteristic changes are seen in REM sleep in depression including:[16]
- Reduced REM sleep latency (individuals have earlier REM sleep)[17]
- Increased REM sleep density (there is greater concentration of REM sleep)[18]
- Decreased sleep efficiency (more time spent awake in bed)
- Decreased slow-wave sleep (meaning decreased N3, or stage 3 and stage 4 sleep)[19]
- More early morning awakenings (terminal insomnia), especially in major depressive disorder with melancholic features
- In general, antidepressants suppress REM sleep and increase REM latency, and thus antidepressants appear to normalize these changes in depression (except bupropion)
Clinical Pearls
- Waking up during the night is not uncommon or pathological. It is the amount time it takes to fall back asleep that affects sleep quality
- Sleep initiation insomnia?
- Ensure there is adequate sleep hygiene, and rule out restless legs syndrome
- Sleep maintenance insomnia?
- Likely intrinsic an intrinsic sleep disorder, and sleep study is likely indicated
- Unusual or problematic behaviours in sleep?
- Sleep study likely required for an accurate diagnosis
- Excessive daytime sleepiness?
- Ensure adequate sleep and rule out an underlying sleep disorder