- Last edited on September 4, 2023
Progressive Supranuclear Palsy (PSP)
Primer
Progressive Supranuclear Palsy (PSP) is a rare neurodegenerative disorder characterized by early postural instability, leading to falls, and a characteristic vertical supranuclear-gaze palsy on physical exam. It is classified as an atypical parkinsonian syndrome (or Parkinson's Plus).
Epidemiology
Prognosis
- Individuals with PSP typically have a prognosis of living another 8 years of onset of first symptoms, but can live as long as 17 years.[3]
Comorbidity
- Individuals with PSP may often have gait abnormalities, muscle weakness, falls, speech difficulties, swallowing difficulties, dysphagia, and urinary tract infections.
- Hypertension is common in individuals with PSP (around 50%).
Risk Factors
- Age is the only known risk factor for PSP.
Diagnostic Criteria
NINDS-SPSP Criteria
The “classic” form of PSP is also called Richardson PSP phenotype (PSP-RS) (also known as Steele-Richardson-Olszewski syndrome). Patients report early difficulties with vertical gaze and pseudobulbar palsy, nuchal dystonia, and dementia. The National Institute of Neurological Disorders and Stroke and Society for PSP (NINDS-SPSP) criteria are the most widely used criteria for the diagnosis of PSP.[4]
NINDS-SPSP PSP Criteria
Litvan, I., et al. Clinical research criteria for the diagnosis of progressive supranuclear palsy (Steele-Richardson-Olszewski syndrome) report of the NINDS-SPSP international workshop. Neurology 47.1 (1996): 1-9.| Symptoms | |
|---|---|
| Probable PSP | Vertical supranuclear gaze palsy plus postural instability and falls within the first year of symptom onset to diagnosis. |
| Possible PSP | Supranuclear gaze palsy or a combination of slow vertical saccades and postural instability with falls within the first year. |
MDS Criteria
The International Parkinson and Movement Disorder Society (MDS)-endorsed PSP Study Group set out to provide an evidence and consensus-based revision of the NINDS-SPSP criteria in 2017, with a much more comprehensive set of criteria.[5]
Basic Features: Core Inclusion and Exclusion Criteria
Höglinger, Günter U., et al. Clinical diagnosis of progressive supranuclear palsy: the movement disorder society criteria. Movement Disorders 32.6 (2017): 853-864.| Mandatory inclusion criteria | 1. Sporadic occurrence 2. Age 40 or older at onset of first PSP-related symptom 3. Gradual progression of PSP-related symptoms |
|---|---|
| Mandatory exclusion criteria | Clinical findings 1. Predominant, otherwise unexplained impairment of episodic memory, suggestive of Alzheimer's Disease (AD) 2. Predominant, otherwise unexplained autonomic failure, e.g., orthostatic hypotension (orthostatic reduction in blood pressure after 3 minutes standing 30 mm Hg systolic or 15 mm Hg diastolic), suggestive of multiple system atrophy or Lewy body disease 3. Predominant, otherwise unexplained visual hallucinations or fluctuations in alertness, suggestive of dementia with Lewy bodies 4. Predominant, otherwise unexplained multisegmental upper and lower motor neuron signs, suggestive of motor neuron disease (pure upper motor neuron signs are not an exclusion criterion) 5. Sudden onset or step-wise or rapid progression of symptoms, in conjunction with corresponding imaging or laboratory findings, suggestive of vascular etiology, autoimmune encephalitis, metabolic encephalopathies, or prion disease 6. History of encephalitis 7. Prominent appendicular ataxia 8. Identifiable cause of postural instability, e.g., primary sensory deficit, vestibular dysfunction, severe spasticity, or lower motor neuron syndrome Imaging findings 1. Severe leukoencephalopathy, evidenced by cerebral imaging 2. Relevant structural abnormality, e.g., normal pressure or obstructive hydrocephalus; basal ganglia, diencephalic, mesencephalic, pontine or medullary infarctions, hemorrhages, hypoxic-ischemic lesions, tumors, or malformations |
Core Clinical Features
Höglinger, Günter U., et al. Clinical diagnosis of progressive supranuclear palsy: the movement disorder society criteria. Movement Disorders 32.6 (2017): 853-864.| Levels of Certainty | Ocular Motor Dysfunction | Postural Instability | Akinesia | Cognitive Dysfunction |
|---|---|---|---|---|
| Level 1 | O1: Vertical supranuclear gaze palsy | P1: Repeated unprovoked falls within 3 years | A1: Progressive gait freezing within 3 years | C1: Speech/language disorder (i.e. - nonfluent/agrammatic variant of primary progressive aphasia or progressive apraxia of speech) |
| Level 2 | O2: Slow velocity of vertical saccades | P2: Tendency to fall on the pull-test within 3 year | A2: Parkinsonism, akinetic-rigid, predominantly axial, and levodopa resistant | C2: Frontal cognitive/behavioural presentation |
| Level 3 | O3: Frequent macro square wave jerks or “eyelid opening apraxia” | P3: More than two steps backward on the pull-test within 3 years | A3: Parkinsonism, with tremor and/or asymmetric and/or levodopa responsive | C3: Corticobasal syndrome |
Signs and Symptoms
- On cognitive testing, letter fluency is worse than semantic fluency (versus in Alzheimer's, where semantic fluency is worse than letter fluency).[6]
- Pseudobulbar signs may be present, and retropulsion is often prominent.
- Patients typically have an early history of falls and difficulty with rising from chairs.
- Spontaneous new episodes of anxiety or new psychiatric diagnoses in late life has been reported in cases of PSP.[7]
- Some individuals may have been treated as a primary psychiatric disorder (e.g. - late onset anxiety) for several years before being formally diagnosed with PSP, and may only come first in contact with psychiatric specialists.
- Cognitive testing will show psychomotor slowing, poor working memory, and executive dysfunction.
- Reduced cognitive processing speed is considered a hallmark of PSP.[8]
- Common psychiatric symptoms include apathy, depression, sleep disturbances, and disinhibition.[9]
- Rarely, there can be hallucinations or delusions, but this may also be related to the use of dopaminergic agents in these individuals.[10]
- Aphasia, including anomnia, and slowed speech can be a common feature of PSP, and as severe as the primary progressive aphasias.[11]
Pathophysiology
- The major genetic risk factor for sporadic PSP is a common variant in the gene encoding microtubule-associated protein tau (MAPT)
- There is ontracerebral aggregation of MAPT, which predominantly involves isoforms of the four microtubule-binding repeats (4R) tau
- The definite diagnosis of PSP requires a post-mortem neuropathological examination.
Differential Diagnosis
The differential diagnosis for PSP is very broad and includes:[12]
- Neurodegenerative
-
- Since PSP and corticobasal degeneration are both Four-repeat (4R) tauopathies, these two neurodegenerative disorders may be confused in the initial stages.
- Heredodegenerative
- Kufor Rakeb disease
- Perry syndrome
- Mitochondrial disease (POLG)
- Dentatorubral pallidoluysian atrophy
- Gaucher disease
- Neuroacanthocytosis
- Vascular
- Vascular-Progressive supranuclear palsy (Vascular-PSP)
- Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL)
- Infectious
- Whipple’s disease
- Immune-mediated
- Paraneoplastic encephalitis (Anti-Ma1, Anti-Ma2 antibodies)
Physical Exam
Ocular Findings and Vertical Gaze Palsy
PSP with Vertical Gaze Palsy, Abnormal Optokinetic Nystagmus and Inability to Suppress Blinking to Light
PSP with Vertical Gaze Palsy, Abnormal Optokinetic Nystagmus and Inability to Suppress Blinking to Light- When examined with an optokinetic flag, there is slowing of vertical saccades (upwards and downwards) and also loss of the upward and downward fast phase.
- These are commonly early signs in PSP, and often precedes the development of the onset of full on downgaze or vertical palsy.[13]
- Patients with PSP also tend to to have difficulty suppressing blinks when a bright light is shone into the eyes, this is a frontal release sign similar to the glabellar reflex, which can be present in Parkinson's disease.
Motor
- As per the diagnostic criteria, patients typically have more axial rigidity
Other Signs
- The “Applause sign” may help discriminate PSP from Frontotemporal Dementia (FTD) and Parkinson's Disease (PD). To elicit the sign, patients are asked to clap
3times. If they clap more than 3 times, it is a positive sign.[14] - There may also be a so-called “dirty-tie sign,” because individuals cannot see that they are dropping food when they eat.
- However, more recent studies have suggested that the applause sign should be interpreted as a merely a sign of frontal lobe dysfunction, and that it can be found in FTD and AD.[15]
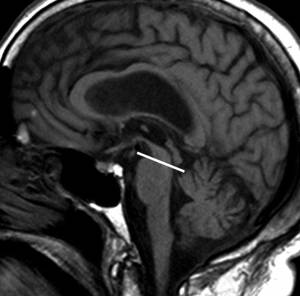
Neuroimaging
MRI
Differentiation of PSP from Parkinson's disease (PD) and Multiple System Atrophy (MSA) can be difficult, particularly in the early stages of the disease. The hummingbird sign (also known as the penguin sign) refers to the appearance of the midbrain in patients with progressive supranuclear palsy (PSP).[16][17][18][19]
Treatment
- If there are features of parkinsonism, some patients may benefit from a levodopa trial.