- Last edited on February 9, 2024
QT (QTc) Prolongation and Monitoring
Primer
QT (QTc) Prolongation is associated with many psychotropic medications (especially antipsychotics) and some are linked to serious ventricular arrhythmias (e.g. - Torsades de Pointes) and sudden cardiac death. The risk of QT prolongation is likely dose-related, but the overall absolute risk is low. ECG monitoring is recommended for all patients on QT-prolonging agents, especially those taking medications long-term. There are few guidelines on the monitoring of QT, but it is generally recommended when a QT-prolonging agent is started, or if there are there is a dose increase. Yearly monitoring is suggested by some guidelines.
Why is QT prolongation bad?
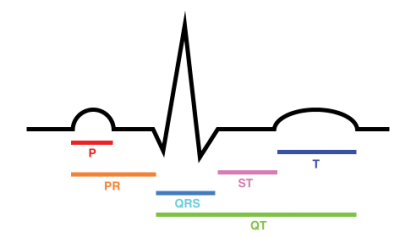
The QT interval indicates the length of cardiac repolarization (the time for the ventricles to contract and relax). Simply put, an increase in the QT interval causes heterogeneity in electrical phasing in different ventricular structures of the heart. This can cause events like ventricular extrasystole and Torsades de Pointes, leading to ventricular fibrillation and sudden death.[1]QT interval
The QT interval is an interval between the start of the QRS complex to the end of the T Wave on an electrocardiocgram (in milliseconds).
QT Correction (QTc)
Since different heart rates can affect the QT interval, the QT interval is usually reported as the QTc (QT corrected for heart rate). There are 4 types of formulae to correct the QT interval, mainly Bazett, Fredericia, Framingham, and Hodges. Each type of correction formula can give markedly different QTc values.
The Bazett correction (which is most commonly used and found in most preprogrammed ECG machines that calculate the QTc), however, it tends to:
- Overestimate QTc interval in tachycardia
- Underestimate the QTc interval in bradycardia
This overcall can lead to unnecessary withholding of first-line medications. Thus manual measurement using the Fredericia or Framingham corrections, or population-based nomograms have the best rate correction. These alternative methods are recommended for patients starting new drugs or on shorter regimens.[2]
Beyond QTc
Regardless of the different corrections, the QTc remains an imprecise indicator of risk of Torsades de Pointes and cardiac mortality. Combining QTc with T-wave morphology better predicts the risk for Torsades de Pointes. Some patients whose QTc falls above the traditional upper limits can also take medications that alter cardiac repolarization without developing Torsades.[3]
QTc Ranges
Different clinical guidance exists for the cut off scores for QTc intervals (which also depend on correction methods). Below are two guidelines to guide decision making.
Management of QT Prolongation
Adapted from: Taylor, D. M., Barnes, T. R., Young, A. H. (2018). The Maudsley prescribing guidelines in psychiatry.| QTc* (men) | QTc* (women) | Action | Cardiology Referral |
|---|---|---|---|
| <440 ms | <470 ms | None unless abnormal T‐wave morphology | No |
| 440 to 500 ms | 470 to 500 ms | Consider reducing dose or switching to drug of lower effect and repeat ECG | Consider |
| >500 ms | >500 ms | Repeat ECG. Stop suspected QT-prolonging agents(s) and switch to drug less QT effects | Yes |
Management of QT Prolongation
Adapted from: Funk, M. C. et al. (2020). QTc prolongation and psychotropic medications. American Journal of Psychiatry, 177(3), 273-274.| QTc* (men) | QTc* (women) | Interpretation |
|---|---|---|
| <430 ms | >450 ms | Normal |
| 431 to 470 ms | 451 to 480 ms | Borderline |
| >470 ms | >480 ms | Prolonged |
Risk Factors
Risk factors for QT prolongation include:
- Female gender
- Use of medications primarily metabolized by CYP 3A4 (e.g. - citalopram, quetiapine), due to risk for greater drug-drug interactions from potent inhibitors of CYP 3A4 (e.g. - grapefruit juice, antivirals, antibiotics), which may inadvertently contribute to an increased dose of QTc prolonging drugs.[4]
- Older age (>65 years old)
- Eating disorders
- Heart disease (recent myocardial infarction, congestive heart failure, bradyarrhythmias)
- Electrolyte disturbances (hypokalemia and hypomagnesia)
- Renal impairment (CrCl <20ml/min)
Other Factors That Affect QTc
- There is normal physiological variation in the QTc interval. QT can vary with gender, time of day, food intake, alcohol intake, menstrual cycle, ECG lead placement
- Plasma levels can also change QTc prolongation is most prominent at peak drug plasma levels and least obvious at trough levels.
QT-prolonging Medications
The list of medications here will focus on psychotropic medications. Non-psychotropic medications that also affect QT include: antibiotics, antimalarials, and antiarrhythmics.
Antipsychotics
Antipsychotics
Adapted from: Taylor, D. M., Barnes, T. R., Young, A. H. (2018). The Maudsley prescribing guidelines in psychiatry.| No effect | • Brexpiprazole • Cariprazine • Lurasidone |
|---|---|
| Low effect | • Aripiprazole*[5] • Asenapine • Clozapine • Flupenthixol • Fluphenazine • Loxapine • Perphenazine • Paliperidone |
| Moderate effect | • Amisulpride • Risperidone • Olanzapine • Quetiapine • Haloperidol • Chlorpromazine |
| High effect | • Risperidone |
| Unknown | • Zuclopenthixol |
Antidepressants
Antidepressants
Adapted from: Taylor, D. M., Barnes, T. R., Young, A. H. (2018). The Maudsley prescribing guidelines in psychiatry.| None | • Agomelatine • Bupropion • Fluoxetine* • Duloxetine*[6][7] • Fluvoxamine*[8] • MAOIs • Mirtazapine • Moclobemide • Vilazodone • Reboxetine • Paroxetine*[9] • Sertraline*[10] • Vortioxetine |
|---|---|
| Low effect | • Trazodone |
| Moderate effect | • Citalopram • Escitalopram • Venlafaxine |
| High effect | • Tricyclics |
Opioids
| High effect | • Methadone |
|---|
Methadone
Methadone, either alone or combined with other QT‐prolonging agents, can cause QT interval prolongation. Patients on more than 100mg of methadone daily should be closely monitored as the risk of QTc prolongation is dose related.
Substances
Cocaine is also a QT‐prolonging agent.
Management
Medications
- If on antidepressant, try switching to → bupropion, SSRIs other than citalopram/escitalopram
- If on antipsychotic, try switching to → aripiprazole, or lurasidone
- If on methadone, try switching to → buprenorphine, Suboxone
- Remove interacting drugs that prolong metabolism and increase plasma levels of QT-prolonging drugs (e.g. - omeprazole can increase plasma levels of escitalopram and citalopram)
Electrolytes
- If the QTc is not normal, i.e. > 500, order Mg and K levels. If these levels are low, then it should be replaced and the ECG repeated again
- Try to keep potassium levels above 4.0, and Mg above 1.0, if you’re worried about QTc prolongation
- Correct underlying bradycardia