Table of Contents
Electroconvulsive Therapy (ECT)
Primer
Electroconvulsive Therapy (ECT) is a form of brain stimulation performed under general anesthesia, in which electrical currents are passed through the brain, intentionally triggering a brief seizure. The indications for treatment with ECT are numerous, including for major depressive disorder, bipolar mania/depression, schizophrenia, and catatonia.
History
During the late 1930s it was observed that people suffering from both epilepsy and serious mental illnesses exhibited an interesting phenomenon in the aftermath of a seizure. These individuals would have a reduction in psychiatric symptoms, lasting anywhere from days to weeks.[1] Based on these observations, seizures were induced in patients who did not otherwise have epilepsy. It was found that the safest way to accomplish this was by delivering an electrical shock to the head.
A Dark History
ECT was used extensively and indiscriminately in the first three decades of it discovery, due to the lack of psychiatric medications at the time (the pre-antipsychotic and antidepressant era). This indiscriminate use came with serious complications and valid concerns. The public perception of ECT later became characterized in numerous movies (e.g. - One Flew Over The Cuckoo's Nest), and was portrayed as an inhumane, horrific, and frightening procedure. This exaggerated portrayal in popular culture unfortunately stigmatized an effective and often life-saving procedure when used in the right patients with serious mental illness.Current Practice
Today, ECT is used effectively to treat various psychiatric disorders, including severe mood disorders (i.e. - severe depression with melancholic features, psychotic depression, and severe, acute mania). Techniques and safety protocols for administering ECT have also changed dramatically. ECT is now an anesthetic procedure, and requires the use of general anesthesia and muscle relaxants. The patient is therefore fully anesthetized and asleep during the procedure. Serious or persistent side effects now extremely rare. Although, ECT is often considered a treatment of last resort, in most jurisdictions, it remains under-utilized due to stigma. ECT can be extremely effective and, at times, a life-saving procedure. ECT remains a first-line treatment for many psychiatric disorders.[2]
Indications
Indications for ECT include:
- Treatment-refractory mania
- Major depressive disorder (unipolar or bipolar depression)
- ECT is generally recommended as a second-line treatment for major depressive disorder because of the increased risk for adverse events.
- However, ECT can also be used as a first-line treatment in certain clinical situations including: acute suicidal ideation, psychotic features, treatment-resistant depression, repeated medication intolerance, catatonic features, prior favourable response to ECT, rapidly deteriorating physical status, during pregnancy (for any of the above indications), and patient preference.[3]
- Refractory obsessive-compulsive disorder (OCD)
- Refractory psychosis, from schizophrenia or schizoaffective disorder
- Refractory status epilepticus[5]
- Severe suicidality
Contraindications
- Relative contraindications include:
- Space-occupying cerebral lesion with increased intracranial pressure or mass effect
- Recent myocardial infarction (if <
1month ago) - Recent stroke or cerebral hemorrhage (if <
1month ago) - Unstable vascular aneurysms or malformations
- Pheochromocytoma
- Class 4 or 5 anaesthesia risk (ASA IV, ASA V)
- Recent orthopedic injury with unstable fracture/dislocation (if <
1month ago)
Mechanism of Action
- ECT delivers an electrical stimulus, which induces an action potential in the neurons in the brain.
- The exact mechanism of action of ECT's antidepressant effects remains unknown, but it is hypothesized that the induced seizure leads to changes in neurotransmitters, neuroplasticity, functional connectivity, increased levels of brain-derived neurotrophic factor (BDNF), hormones, and/or neuropeptides.[8]
- The seizure event itself, not the method of induction, is the essential element in the efficacy of ECT.[9]
Physiological Effects
Cardiac
- ECT affects autonomic nervous system activity, which causes rapid hemodynamic changes. The heart rate goes down (as ECT causes a parasympathetic drive). The effects of ECT on the heart is similar to a brief period of “vigorous exercise.”[10]
Brain
- During ECT, cortical blood flow increases by up to 300%, which increases intracranial pressure (ICP). Cerebral oxygen demand also increases up to 200% during seizure activity. ECT remains safe in patients with brain tumours and intracranial masses provided that there is not significant cerebral edema (Hence, increased ICP is a relative contraindication).[11] Brain volumes increase with ECT treatment,[12] and there is also an increase in Brain Derived Neurotrophic Factor (BDNF) levels.[13][14] During ECT, the brain will try to achieve homeostasis in response to the electrical current, and will release GABA to suppress seizures.[15] The release of GABA is thought to play a role in the antidepressant effect of ECT as well.
Pre-ECT
Informed Consent
It is important to inform patients about the risks and benefits of ECT. Below is a template for informed consent:
- Ask patient what they understand about ECT
- Explain procedure (# of treatments, what treatments will consist of, what happens just before and after treatment, how they will feel, how long each session lasts)
- Explain efficacy (with depression, bitemporal is 65%, RUL is 58%)
- Cover serious/life threatening risks (1 per 10,000 treatment deaths, risks of general anesthesia)
- Cover common side effects (confusion, headache, muscle pains, HTN, cardiac changes, nausea, cognitive difficulties - specifically memory 1-2 months prior and after procedure may be “hazy”)
- Discuss alternate treatment medications (continue with medications, change medications, psychotherapy options)
- Discuss next steps (work-place adjustment, change to medications prior to treatment course beginning)
- Limitations with treatment (no driving for 24 hours, time off work/school)
Medications
Some medications should be stopped prior to starting ECT, while others should be continued.
Medication indications and contraindications
| Medications to continue | Medications to stop or hold |
|---|---|
| Antihypertensives (reduce hypertension during procedure) | Anticonvulsants (taper dose, or discontinue completely) |
| Heartburn medications (e.g., proton pump inhibitors, H2 blockers) (reduce gastric secretions and the risk of aspiration) | Stimulants (taper and discontinue completely) |
| Glaucoma medications | Lithium (discontinue 36-48 hours prior to treatment, because there is a risk of developing delirium while on lithium and receiving ECT) |
| Antipsychotics (Haloperidol, clozapine, risperidone - may be beneficial in combination with ECT) | MAOIs (consider dose reduction) |
| Antidepressants | Benzodiazepines (should be held by 17:00, the day before each ECT treatment) |
| Bronchodilators (to optimize their respiratory function for the procedure) | Diuretics (hold in the morning to help prevent patients from having episodes of urinary incontinence during the procedure) |
Procedure
Checklist
1. Confirm and Check
- Confirm ID of patient (name, age, patient diagnosis)
- Let anesthesia know of medication doses
- Assess patient for symptoms since the last treatment
- Ensure patient is NPO at least 8 hours prior to treatment
- Confirm ECT parameters
- Set parameters on the machine
- Obtain BP/HR/O2 sat/ECG monitoring
- Prep skin and scalp
- Prep ECT electrodes
- Place EEG monitoring electrodes appropriately
2. Anesthesia
- Anesthesia to obtain IV access
- Anesthesia to administer IV meds
- Anesthesia to pre-oxygenate
3. Muscle relaxant
- Ensure appropriate muscle relaxant (wait at least 60 seconds from the administration of succinylcholine)
4. Placement
- Anesthesia to place bite block
- Place ECT electrodes
5. Electrical stimulus
- Administer stimulus
6. Seizure
- Monitor motor seizure activity (time, strength)
- Monitor EEG seizure (time, resolution, post-ictal suppression)
- Anesthesia to ensure appropriate oxygenation, with suction of airway if necessary
7. Post-ictal recovery
- Administer any post-treatment medications
- Monitor vitas post-treatment
- Observe patient for 1 hour post-treatment
- Ensure patient is accompanied home once recovery monitoring complete
- Ensure documentation complete
Parameters
Treatment parameters for ECT include:
- Electrode placement and position
- Electrical intensity/stimulus
- Pulse width
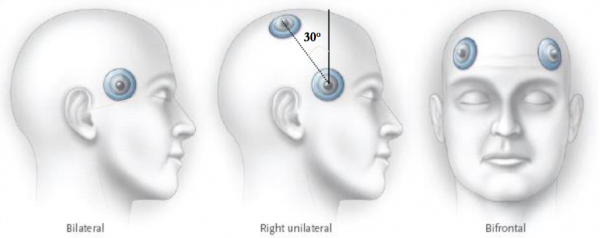
Electrode Placement
Electrode Placement Tip
- Use concave electrode plates for bifrontal (BF) and right unilateral (RUL)
- Use flat electrode plates for bitemporal (BT)
- ECT can be delivered via one of 3 placements: right unilateral placement (RUL), bifrontal (BF), or bitemporal (BT).
- Right unilateral (also called the D'Elia placement) ECT is typically tried first due to its more favourable cognitive profile. Right unilateral ECT is also preferred over left unilateral, since most individuals are left-hemisphere dominant. Left unilateral ECT can be considered in patients if cognitive sparing of right hemispheric function (especially visual-spatial) is important for their livelihood.
- If unilateral ECT fails after 6 to 10 treatments, or there is a history of treatment failure, then one should consider moving onto bilateral ECT.
- Bifrontal ECT may be as effective as bitemporal, but is more cognitively advantageous.
- Bitemporal ECT has a greater incidence of anterograde and retrograde amnesia. Ultimately, bilateral ECT should be used if there is greater urgency for improvement or life threatening situations.
ECT Electrode Placement
Adapted from: Rapoport, M. J. (2016). Geriatric psychiatry review and exam preparation guide: A case-based approach.| Placement | Advantages | Disadvantages |
|---|---|---|
| Right Unilateral (RUL) | • Response rates comparable to BT and BF • Ultrabrief pulse width ECT has good evidence for benefit • Fewer cognitive side effects • Good for patients with cognitive impairment while receiving bilateral ECT, or a history of cognitive side effects with bilateral ECT | • Need higher dosages (4-6x seizure threshold), so may not be able to deliver therapeutic dose for elderly with high seizure thresholds • Slower response than with bilateral placement |
| Bifrontal (BF) | • Faster response than RUL • Possibly fewer cognitive side effects compared to BT in elderly patients | • More cognitive side effects compared to RUL |
| Bitemporal (BT) | • Faster response than RUL • Considered gold standard • Good for patients who need rapid response | • More cognitive side effects compared to RUL |
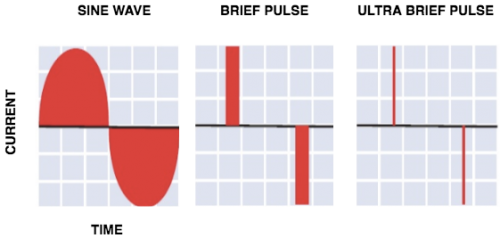
Electrical Stimulus
- The electrical intensity is based on the minimum intensity to produce a generalized seizure, called the seizure threshold (ST)
- Before the invention of newer techniques, older sine wave machines were used, which delivered long pulse width, and was associated with greater side effects.
- Now, brief pulse (BP) or ultra brief pulse (UBP) (i.e. - a pulse width < 0.5 ms) ECT is used, which provides a more efficient delivery of electrical energy with less side effects (see figure 2).
- The amount of electrical stimuli delivered depends on the placement of the electrodes.
- The electrodes can be bifrontal, bilateral, or right unilateral (RUL) (see figure 1).
- Typically, RUL is used because it results in less cognitive side effects.
- The delivered electrical pulse is recommended to be:
- 6 times above the seizure threshold for patients receiving RUL ECT, and
- 2 times above the seizure threshold for BF or BT ECT.[16]
- Higher age is associated with a higher seizure threshold, and stimulus intensity may need to be increased for these individuals.[17]
Recommendations for Delivery of Electroconvulsive Therapy
Milev, R. V. et al. (2016). Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: section 4. Neurostimulation treatments. The Canadian Journal of Psychiatry, 61(9), 561-575.| 1st line | • Brief pulse RUL (at 5-6× seizure threshold) • Brief pulse BF (at 1.5-2.0× seizure threshold) |
|---|---|
| 2nd line | • Ultrabrief pulse RUL (up to 8× seizure threshold) or ultrabrief pulse BF (at 1.5-2× seizure threshold) • Brief pulse BT (at 1.5-2× seizure threshold) |
| 2nd line | • Twice weekly ECT sessions have similar efficacy to thrice weekly but have longer duration of treatment |
| 2nd line | • If no response to RUL after 4 to 6 treatments, switch to bilateral ECT (BT or BF) |
| 2nd line | • For maintenance pharmacotherapy post-ECT, use an antidepressant that has not been tried prior to ECT or nortriptyline plus lithium or venlafaxine plus lithium. • Maintenance use of ECT is as effective as pharmacotherapy in preventing relapse/recurrence after an acute course of ECT. |
Seizure Duration
- An adequate seizure in ECT is one that lasts around or greater than
30seconds. - If the seizure duration is less than this, there are several things to consider:
- If it is a brisk seizure with prominent motor activity, a higher dose of succinylcholine should be considered
- Review which anesthetic agents the patient is on, and the potential effects on seizure duration
- If there is a poor seizure response, you can consider:
- Using hyperventilation to augment the seizure duration[18]
- During the next ECT session, you can also suggest the following:
- Increase hydration
- Administering caffeine to increase the duration of seizures[19]
Medications and Impact on Seizure Duration
| Increased seizure duration | Etomidate, ketamine,[20] caffeine |
|---|---|
| No effect | Methohexital, remifentanil, alfentanil |
| Shortened seizure duration | Propofol, midazolam, lorazepam, thiopental, thiamylal, lidocaine |
Post-ECT
Response
- ECT has the best response rate in geriatric depression, patients with a greater severity of illness, psychotic depression, and when there is an absence of personality disorders.
- In individuals with borderline personality disorder, the rates of ECT response are significantly lower, and this is an important risk/benefit consideration that needs to be discussed with patients.[21]
- The effects of ECT are also dose-dependent, with a better response at higher doses.[22]
- Patients can expect improvement in symptoms by the third treatment, and achieve remission beginning by the seventh treatment.[23] Suicidal ideation also similarly decreases greatly by around the fourth treatment.[24] ECT also improves quality of life measures significantly for patients post-treatment.[25]
- The best and strongest predictor of non-response to ECT is the degree of non-response to previous antidepressant medications. Response rates are about 50% in those who have treatment-resistant depression and up to 90% in treatment-naive patients.[26]
Number of Treatments
- ECT treatment ranges between 6 to 18 treatments, and can be delivered 2 to 3 times per week.
- Administering ECT only 2 times per week confers a better cognitive profile.
- More than 3 treatments per week are not recommended, as they are associated with higher frequency of cognitive side effects.
- If after 12 sessions there is no response, no further ECT should be pursued.
Follow Up Treatment
- About 50% of patients will relapse with depressive symptoms at the 12-month mark, even after a successful course of ECT.[27]
- Patients who receive ongoing antidepressant pharmacotherapy reduce their relapse rate by approximately half compared to patients who do not have any treatment post-ECT.[28]
- Post-ECT pharmacotherapy should be continued for at least 12 to 24 months. Antidepressant choice should be the one that the patient responded the best to in the past. In absence of an effective antidepressant, nortriptyline plus lithium, or venlafaxine plus lithium is recommended.[31]
Maintenance ECT
- Maintenance ECT (“prophylactic ECT”) should be added after an individual has gone through a second course of ECT. In addition to maintenance ECT, augmentation with an antidepressant, plus lithium should be considered.[32]
- The most commonly used maintenance ECT schedule involves weekly treatments for 4 weeks, then biweekly for 8 weeks, and then monthly treatments. If signs of relapse occur, more frequent treatments should be given.[33]
Side Effects and Adverse Events
Possible side effects and adverse events during ECT and post-ECT include:
Common and Rare ECT Side Effects and Adverse Events
| Phase of ECT | Incidence | Notes | |
|---|---|---|---|
| Transient asystole | During procedure | 65.8%[36] | Older patients are actually less likely to experience this than younger patients. Considered self-limiting and not associated with any untoward outcomes.[37] |
| Bradycardia | During procedure | Common | Self-limiting. Very rare case reports of bradycardia persisting post-ECT.[38] |
| Transient hypertension | During procedure | Up to 67% in patients over age 85 | Self-limiting. |
| Dental injury, orobuccal lacerations | During procedure | 0.02% to 0.3%[39] | Use a bite block prevents this, and overall incidence is very rare. |
| Headaches | Post-procedure | 45% | Typical over the counter pain medications can be used to address this. Rocuronium should be considered over succinylcholine for patients with prominent myalgia and headaches |
| Myalgia | Post-procedure | 20% | Note that muscle aches and pain is due to succinylcholine from anesthesia, not the ECT itself. |
| Jaw pain | Post-procedure | Common | Due to contraction of masseter muscle due to direct electrical contraction |
| Falls | Post-procedure | • 14% (age 65 to 80)[40] • 36% (age >80) | Having a falls prevention plan and follow up is important in older adults. Less of a concern in younger patients. |
| Nausea and vomiting | Post-procedure | 1 to 25% | Can give ondansetron post-ECT for management. |
| Post-ictal confusion | Post-procedure | 10%[41] | Typically lasts 15-60 minutes post-ECT, and self-limiting. However, any episodes lasting >60 minutes should be treated as a post-ictal delirium, and all ECT treatments should be held! |
| Manic switch | Post-procedure | 7%[42] | These individuals may have a history of bipolar disorder or hypomanic episodes. |
Memory and Cognition
- Cognition is a broad term that encompasses several components, including: attention, anterograde memory (ability to remember new information), retrograde memory (ability to remember past memory), procedural memory, and reaction time.
- Memory loss (both retrograde and anterograde) is a known side effect from ECT, particularly around the time of ECT treatment:[43]
- Subjective memory worsening is reported by a minority of patients, and those at greatest risk are:
- Young women[44]
- Individuals with prexisting cognitive impairment
- Older adults
- Those receiving bitemporal ECT
- More frequent ECT administration (i.e. - 2 sessions per week vs. 3 sessions)
- Use of lithium during ECT treatment
- Higher anesthetic doses
- The amnestic effects of ECT are greatest and most persistent for knowledge about the world (impersonal memory) compared with knowledge about the self (personal memory).
- Overall, ECT is associated with short-term cognitive effects, but cognition eventually returns or surpasses their pre-ECT baseline.[45]
- The majority of evidence suggests that ECT given over a period of years will not cause cumulative cognitive deficits.
- There are also reduced rates of dementia in geriatric patients with mood disorders who receive ECT.
- Importantly, this means ECT does not increase the risk of dementia in the elderly, making it a safe and appropriate option.[46]
- It is important to note however, in rare cases, some individuals can experience significant and distressing memory loss, and this remains an under-researched area in ECT.
- If there are cognitive side effects from ECT, you can try to:
- Reduce the frequency of treatments (i.e. - 3× per week to 2× per week)
- Reduce the electrical stimulus intensity during treatment
Safety and Mortality
- Overall, ECT is very safe and rapid acting. Out of all medical procedures involving anesthesia, it is the lowest risk procedure.[47]
- The mortality rate from ECT has been estimated to be less than 1 death per 98,000 treatments, which is similar to the background rate associated with anesthetic induction for any surgical procedure.[48]
- Several studies have shown overall lower all-cause mortality in those who receive ECT:
- One study showed a lower overall mortality rate from natural causes in inpatients who have received ECT compared to those who did not.[49]
- A 2022 retrospective study showed no evidence for a clinically significant increased risk for serious medical events with exposure to ECT, and the risk of suicide was in fact found to be significantly reduced compared to the non-ECT group.[50]
- In one study, older adults with geriatric depression, those who ECT treatment had overall lower mortality than those on antidepressants.[51]
Brain Damage
- No clinical studies have shown damage to the brain structures related to ECT.[52]
Comparison with Other Brain Stimulation Therapies
Depression
Neurostimulation in the Treatment of Major Depressive Disorder
Milev, R. V. et al. (2016). Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: section 4. Neurostimulation treatments. The Canadian Journal of Psychiatry, 61(9), 561-575.| Neurostimulation | Overall Recommendation | Acute Efficacy | Maintenance Efficacy | Safety and Tolerability |
|---|---|---|---|---|
| rTMS | • First line (for patients who have failed at least 1 antidepressant) | Level 1 | Level 3 | Level 1 |
| ECT | • Second line • First line in some acute clinical situations | Level 1 | Level 1 | Level 1 |
| tDCS | • Third line | Level 2 | Level 3 | Level 2 |
| Vagal Nerve Stimulation (VNS) | • Third line | Level 3 | Level 2 | Level 2 |
| DBS | • Investigational | Level 3 | Level 3 | Level 3 |
| MST | • Investigational | Level 3 | Not known | Level 3 |