Table of Contents
Posttraumatic Stress Disorder (PTSD)
Primer
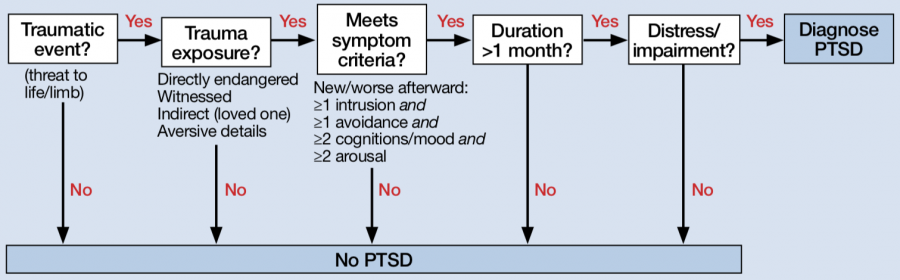
Posttraumatic Stress Disorder (PTSD) is a mental disorder diagnosed after an exposure to trauma, including actual or threatened death, serious injury, or sexual violation. It is characterized by intrusive and distressing memories or dreams, dissociative reactions, and substantial psychological or physiological distress related to the event. A diagnosis of PTSD requires evidence of exposure to trauma, and is characterized by intrusive and dissociative symptoms.
Epidemiology
- The lifetime prevalence of PTSD is around 6-9%, and up to 30% in US Vietnam War veterans.[1]
- Rates are also higher in emergency service personnel, including fire fighters, police officers, and paramedics
- Survivors of rape, military combat, captivity, and wars are also at increased risk.[2]
- It is more frequent in women than in men (2:1), with an onset generally in the mid to late 20s. PTSD is associated with high rates of functional impairment, somatic complaints, suicide risk, and comorbid psychiatric disorders.
Prognosis
- PTSD can occur at any point in life, beginning after age 1.[3]
- Symptoms usually begin within the first 3 months after trauma, although for some there may be a delay of months or years before the criteria for a full diagnosis is met.
- However, individuals generally have substantially improved occupational functioning at work, relationships, and social interactions.[6]
- Long-term employment disability related to PTSD is also rare. In general, clinicians and patients should expect that functioning will improve significantly over the long term, even if posttraumatic stress symptoms remain.
Comorbidity
- Individuals with PTSD and 80% more likely than those without PTSD to meet criteria for another mental disorder, including depressive disorders, anxiety disorders, substance use disorders (in particular alcohol use disorder), and borderline personality disorder.
- Individuals with comorbid borderline personality disorder and PTSD have a greater risk for suicide than individuals with either diagnosis alone.
- Close to half of individuals seeking substance use disorder treatment also meet criteria for current PTSD, and individuals with co-occurring disorders tend to have poorer treatment outcomes compared with those without such comorbidity.
- Substance use disorder and conduct disorder is more common among males with PTSD than females
- Recent data from veterans in the Afghanistan and Iraq wars, have found that PTSD and mild traumatic brain injuries had a cooccurrence of 48%.
- In children with PTSD, oppositional defiant disorder and separation anxiety disorder are the predominant comorbidities.
Risk Factors
- Epidemiological research on PTSD has shown consistently that pre-existing psychopathology is a strong predictor of PTSD following a trauma exposure. Thus, these comorbid conditions should also be treated concurrently with PTSD. Pre-trauma risk factors for developing PTSD include:
- A history of childhood emotional problems, prior mental disorders such as panic disorder, depressive disorder, or obsessive compulsive disorder, and a family history of psychiatric disorders.
- Environmental risk factors include lower socioeconomic status, lower education and intelligence, childhood adversity, and cultural characteristics
- Female gender and certain genotypes may also increase one's risk for PTSD
- Peritrauma factors (risk factors at the time of the trauma) include severity of the trauma, degree of perceived threat to life, personal injury, degree of interpersonal violence, and for military personnel, whether or not they were a perpetrator or witness to a killing of an enemy.
- Temperamental traits such as inappropriate coping strategies and negative appraisals are risk factors.
- Individuals with the support of social networks such as family stability is an important protective factor.
Cultural
- PTSD can be expressed differently in various cultural contexts (similar to panic attacks and panic disorder).[9] Thus, having an understanding of the cultural concepts of disease and mental disorders is important when assessing symptoms in a cultural context.[10]
- In Hispanic individuals, ataque de nervios (“attack of nerves”) is a cultural syndrome used frequently to describe symptoms of intense emotional upset including acute anxiety, anger, or grief, screaming and shouting uncontrollably, attacks of crying, trembling, feeling of heat in the chest rising into the head, and verbal and physical aggression.[11] Some individuals may even report dissociative episodes.
- In Cambodians, “Khyâl attacks” (khyâl cap) or “wind attacks” include palpitations, shortness of breath, dizziness, and cold extremities. Individuals also have other symptoms of anxiety and autonomic arousal such as neck soreness and tinnitus.[12]
DSM-5 Diagnostic Criteria
6 years. For children 6 years and younger, refer to specific alternative criteria.
Criterion A (Exposure)
Exposure to actual or threatened death, serious injury, or sexual violence in at least 1 of the following ways:
- Directly experiencing the traumatic event(s).
- Witnessing, in person, the event(s) as it occurred to others.
- Learning that the traumatic event(s) occurred to a close family member or close friend. In cases of actual or threatened death of a family member or friend, the event(s) must have been violent or accidental.
- Experiencing repeated or extreme exposure to aversive details of the traumatic event(s) (e.g. - first responders collecting human remains or police officers repeatedly exposed to details of child abuse).
Criterion B (Intrusion Symptoms)
Presence of at least 1 of the following intrusion symptoms associated with the traumatic event(s), beginning after the traumatic event(s) occurred:
- Recurrent, involuntary, and intrusive distressing memories of the traumatic event(s). In children older than 6 years, repetitive play may occur in which themes or aspects of the traumatic event(s) are expressed.
- Recurrent distressing dreams in which the content and/or affect of the dream are related to the traumatic event(s). In children, there may be frightening dreams without recognizable content.
- Dissociative reactions (flashbacks) in which the individual feels or acts as if the traumatic event(s) were recurring. (Such reactions may occur on a continuum, with the most extreme expression being a complete loss of awareness of present surroundings.) In children, trauma-specific reenactment may occur in play.
- Intense or prolonged psychological distress at exposure to internal or external cues that symbolize or resemble an aspect of the traumatic event(s).
- Marked physiological reactions to internal or external cues that symbolize or resemble an aspect of the traumatic event(s).
Criterion C (Avoidance)
Persistent avoidance of stimuli associated with the traumatic event(s), beginning after the traumatic event(s) occurred, as evidenced by 1 or all of the following:
- Avoidance of or efforts to avoid distressing memories, thoughts, or feelings about or closely associated with the traumatic event(s).
- Avoidance of or efforts to avoid external reminders (people, places, conversations, activities, objects, situations) that arouse distressing memories, thoughts, or feelings about or closely associated with the traumatic event(s).
Criterion D (Negative Cognition and Mood)
Negative alterations in cognitions and mood associated with the traumatic event(s), beginning or worsening after the traumatic event(s) occurred, as evidenced by at least 2 of the following:
- Inability to remember an important aspect of the traumatic event(s) (typically due to dissociative amnesia and not to other factors such as head injury, alcohol, or drugs).
- Persistent and exaggerated negative beliefs/expectations about oneself, others, or the world (e.g., “I am bad,” “No one can be trusted,” ‘The world is completely dangerous,” “My whole nervous system is permanently ruined”).
- Persistent, distorted cognitions about the cause or consequences of the traumatic event(s) that lead the individual to blame himself/herself or others.
- Persistent negative emotional state (e.g., fear, horror, anger, guilt, or shame).
- Markedly diminished interest or participation in significant activities.
- Feelings of detachment or estrangement from others.
- Persistent inability to experience positive emotions (e.g., inability to experience happiness, satisfaction, or loving feelings).
Criterion E (Changes in Arousal)
Marked alterations in arousal and reactivity associated with the traumatic event(s), beginning or worsening after the traumatic event(s) occurred, as evidenced by at least 2 of the following:
- Irritable behavior and angry outbursts (with little or no provocation) typically expressed as verbal or physical aggression toward people or objects.
- Reckless or self-destructive behavior
- Hypervigilance
- Exaggerated startle response
- Problems with concentration
- Sleep disturbance (e.g., difficulty falling or staying asleep or restless sleep).
Criterion F
Duration (Criteria B, C, D, and E) is more than 1 month.
Criterion G
The disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning.
Criterion H
The disturbance is not attributable to the physiological effects of a substance (e.g. - medication, alcohol) or another medical condition.
Mnemonic
The clinical presentation of PTSD can be remembered by the mnemonicTRAUMA[13]T- Traumatic event (experienced, witnessed, or was confronted, and the person experienced intense helplessness, fear, and horror)R- Re-experiencing (intrusive thoughts, nightmares, flashbacks, or traumatic memories/images)A- Avoidance (emotional numbing, detachment from others, flattening of affect, loss of interest, lack of motivation, and persistent avoidance of things associated with the traumatic experience)U- Unable to function (symptoms cause negative mood, distress, or cause significant impairment in social, occupational, and interpersonal life)M- 1 month of symptoms (at least)A- Arousal increased (insomnia, poor concentration, irritable, angry, startle reflex, hypervigilance)
Specifiers
Specifiers
Specify whether:
- With dissociative symptoms: The individual’s symptoms meet the criteria for PTSD, and the individual experiences persistent or recurrent symptoms of either of the following:
- Depersonalization: Persistent or recurrent experiences of feeling detached from, and as if one were an outside observer of, one’s mental processes or body (e.g. - feeling as though one were in a dream; feeling a sense of unreality of self or body or of time moving slowly).
- Derealization: Persistent or recurrent experiences of unreality of surroundings (e.g. - the world around the individual is experienced as unreal, dreamlike, distant, or distorted).
Specifiers
Specify if:
- With delayed expression: If the full diagnostic criteria are not met until at least
6months after the event (although the onset and expression of some symptoms may be immediate).
Signs and Symptoms
- Following severe and repeated traumatic events, an individual may experience difficulty with regulation of emotion or keeping interpersonal relationships. Dissociative symptoms may also develop.
- Individuals may be engaged in high-risk activities such as dangerous driving, excessive substance use, or self-injurious behaviours.[14]
- The presentation of PTSD can vary greatly.
- In some individuals, the predominant presentation is marked by fear-based re-experiencing of trauma, and behavioural symptoms.
- For other individuals, dysphoria and negative thoughts may be the predominant symptoms.
- Finally, others may have dissociative symptoms as the predominant presentation.[15]
Diagnostic Pearls
- PTSD is unique among the psychiatric diagnoses in that it requires a specific external event as part of the diagnostic criteria. Incorrect application of the trauma exposure criterion (Criterion A) by clinicians and researchers has led to misdiagnosis and erroneously high prevalence rates of PTSD.[16]
- It is important to recognize that for the majority of individuals, exposure to trauma does not result in PTSD. The symptoms from PTSD must be linked temporally and conceptually to the traumatic exposure to qualify as PTSD symptom.
Diagnostic Criteria (6 Years and Younger)
Criterion A
In children 6 years and younger, exposure to actual or threatened death, serious injury, or sexual violence in 1 (or more) of the following ways:
- Directly experiencing the traumatic event(s).
- Witnessing, in person, the event(s) as it occurred to others, especially primary caregivers.
- Learning that the traumatic event(s) occurred to a parent or caregiving figure.
Criterion B
Presence of 1 (or more) of the following intrusion symptoms associated with the traumatic event(s), beginning after the traumatic event(s) occurred:
- Recurrent, involuntary, and intrusive distressing memories of the traumatic event(s).
- Recurrent distressing dreams in which the content and/or affect of the dream are related to the traumatic event(s).
- Dissociative reactions (e.g. - flashbacks) in which the child feels or acts as if the traumatic event(s) were recurring. (Such reactions may occur on a continuum, with the most extreme expression being a complete loss of awareness of present surroundings.) Such trauma-specific reenactment may occur in play.
- Intense or prolonged psychological distress at exposure to internal or external cues that symbolize or resemble an aspect of the traumatic event(s).
- Marked physiological reactions to reminders of the traumatic event(s).
Criterion C
1 (or more) of the following symptoms, representing either persistent avoidance of stimuli associated with the traumatic event(s) or negative alterations in cognitions and mood associated with the traumatic event(s), must be present, beginning after the event(s) or worsening after the event(s):
Persistent Avoidance of Stimuli
- Avoidance of or efforts to avoid activities, places, or physical reminders that arouse recollections of the traumatic event(s).
- Avoidance of or efforts to avoid people, conversations, or interpersonal situations that arouse recollections of the traumatic event(s).
Negative Alterations in Cognitions
- Substantially increased frequency of negative emotional states (e.g. - fear, guilt, sadness, shame, confusion).
- Markedly diminished interest or participation in significant activities, including constriction of play.
- Socially withdrawn behavior.
- Persistent reduction in expression of positive emotions.
Criterion D
Alterations in arousal and reactivity associated with the traumatic event(s), beginning or worsening after the traumatic event(s) occurred, as evidenced by 2 (or more) of the following:
- Irritable behavior and angry outbursts (with little or no provocation) typically expressed as verbal or physical aggression toward people or objects (including extreme temper tantrums).
- Hypervigilance.
- Exaggerated startle response.
- Problems with concentration.
- Sleep disturbance (e.g. - difficulty falling or staying asleep or restless sleep).
Criterion E
The duration of the disturbance is more than 1 month
Criterion F
The disturbance causes clinically significant distress or impairment in relationships with parents, siblings, peers, or other caregivers or with school behavior.
Criterion G
The disturbance is not attributable to the physiological effects of a substance (e.g. - medication or alcohol) or another medical condition.
Screening and Rating Scales
PTSD Scales
| Name | Rater | Description | Download |
|---|---|---|---|
| Clinician-Administered PTSD Scale for DSM-5 (CAPS-5) | Clinician | The CAPS is a 30-item structured interview that is the gold standard in PTSD assessment. It can be used to make a current (past month) diagnosis of PTSD, lifetime diagnosis of PTSD, and assess severity of PTSD symptoms over the past week. | Link |
| PTSD Checklist for DSM-5 (PCL-5) | Patient | The PCL-5 is a 20-item self-report measure that assesses the 20 DSM-5 symptoms of PTSD. The PCL-5 can monitor symptom change during and after treatment, screening individuals for PTSD, help make a provisional PTSD diagnosis. | Link |
Pathophysiology
- The amygdala, hippocampus, and prefrontal cortex are all involved in the stress response. Traumatic stress can be associated with lasting changes in these brain areas. Individuals with PTSD have smaller hippocampal and anterior cingulate volumes, increased amygdala function, and decreased medial prefrontal/anterior cingulate function. Patients with PTSD also show increased cortisol and norepinephrine responses to stress.[17]
- Brain imaging studies have shown alterations in a circuit including medial prefrontal cortex (including anterior cingulate), hippocampus, and amygdala in PTSD.
Differential Diagnosis
-
- In adjustment disorder, the stressor can be of any severity or type and not just a traumatic event as defined by the PTSD criterion. Adjustment disorder should be diagnosed when there is a trauma, but the individual does not meet all other PTSD criteria.
-
- In acute stress disorder, there is a restriction of the duration of symptoms being between 3 days to 1 month following exposure to the traumatic event.
-
- The arousal and dissociative symptoms of panic disorder, and the avoidance, irritability, and anxiety of generalized anxiety disorder are not linked to a specific traumatic event. The symptoms of separation anxiety disorder are clearly related to separation from home or family, rather than to a specific traumatic event.
-
- In OCD, there are also recurrent intrusive thoughts, but these meet the definition of an obsession. Importantly, the intrusive thoughts are not related to an experienced traumatic event. Compulsions are also usually present in OCD, while this is absent in PTSD.
-
- Major depression does not include any intrusion (Criterion B) or avoidance (Criterion C) symptoms.
-
- Interpersonal difficulties that develop after a trauma would suggest PTSD, rather than a personality disorder, which is more long-standing. A detailed psychiatric history can help elicit this difference.
-
- In dissociative amnesia, dissociative identity disorder, and depersonalization-derealization disorder, an experienced trauma with temporal association is not needed. If PTSD criteria are met, the “with dissociative symptoms subtype” of PTSD should be considered.
-
- New onset of somatic symptoms within the context of a traumatic event would suggest PTSD over conversion disorder.
- Psychotic disorders and others
- Flashbacks in PTSD must be distinguished from illusions, hallucinations, and other perceptual disturbances that may occur psychotic disorders, or psychotic symptoms in mood disorders. Other disorders include delirium, substance/medication-induced disorders, and psychotic disorders due to another medical condition.
-
- When a brain injury occurs in the context of a traumatic event (e.g. - traumatic accident, bomb blast, acceleration/deceleration trauma), PTSD can develop. Thus, traumatic brain injury (TBI)-related neurocognitive symptoms and PTSD are not mutually exclusive diagnoses and may occur concurrently. Differentiating between the two may be challenging. One difference is that while reexperiencing and avoidance are seen in PTSD, executive dyusfunction, disorientation and confusion are more specific to TBI.[18]
Investigations
- As clinically indicated.
Treatment
Prevention and Early Intervention
- Meta-analyses currently do not support the widespread use of individual psychological debriefing in reducing the intensity of PTSD symptoms.
- The evidence for group debriefings is unclear at this time, and is still commonly done in first-responder settings (police, fire, ambulance).
- Multisession trauma-focused cognitive behavioural therapy can be helpful for individuals with PTSD or acute stress disorder.[19]
- Thus, screening for and treating appropriate individuals is recommended over debriefing all trauma victims.
- The data on use of pharmacotherapy to prevent PTSD symptoms at the time of trauma is limited.[20]
Acupuncture
- Verum acupuncture has been shown to be effective in reducing PTSD symptoms and enhancing fear extinction in combat veterans.[21]
Psychotherapy
- Both pharmacotherapy and psychotherapy are effective for the treatment of PTSD.
- Research has not conclusively shown either treatment modality to be superior than the other.[22]
- Cognitive behavioural therapy is a first-line treatment for PTSD.[23]
- Cognitive processing therapy (CPT), trauma-focused CBT (TF-CBT), and prolonged exposure (PE) therapy are also effective treatments.[24]
- Written exposure therapy (WET) has also recently been investigated and shown to be non-inferior to CBT and prolonged exposure therapy.
- WET is a brief focused therapy that involves individuals writing about their trauma experiences and paying particular attention to their thoughts and emotions that occurred at the time of the event, without a need for in vivo exposure
- Eye movement desensitization and reprocessing therapy (EMDR) has also emerged as a trauma-focused therapy with effectiveness.
- Following treatment with psychotherapy, benefits can be maintained between 1 to 10 years.
- In children, art therapy, play therapy, and family therapy (without the perpetrators of the trauma) can also be helpful.[25]
Pharmacotherapy
- Treatment should start with either a selective serotonin reuptake inhibitor or a serotonin norepinephrine reuptake inhibitor.
- If there is poor response or tolerability, the patient should be switched to another first- or second-line agent.
- Alternatively, a second-line agent can be added (patients with PTSD may make few gains during treatment, and it is important to preserve even small gains).
- Patients who do not respond to multiple courses of therapy are considered to have treatment-refractory symptoms.
- In these patients, it is important to reassess the diagnosis and consider other comorbid medical and psychiatric conditions that may be affecting response to therapy.
- Some studies are looking into the role of propranolol reduction of chronic PTSD symptoms, but remains under investigation.[26]
- For PTSD-associated nightmares:
- Prazosin can reduce trauma nightmares and improve sleep quality. However, one recent randomized control trial actually found no difference between prazosin and placebo in military veterans with PTSD-associated nightmares.[27][28]
- Doxazosin has been used off-label as well due to its longer half-life, once-daily dosing, improved absorption profile and possible lower risk for unintended adverse hypotensive effects.[29]
Pharmacotherapy for Posttraumatic Stress Disorder
Katzman, M. A. et al. (2014). Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress and obsessive-compulsive disorders. BMC psychiatry, 14(S1), S1.| 1st line | Monotherapy: fluoxetine, paroxetine, sertraline†, venlafaxine XR |
|---|---|
| 2nd line | Monotherapy: fluvoxamine, mirtazapine, phenelzine |
| 3rd line | Monotherapy: amitriptyline, aripiprazole, bupropion SR, buspirone, carbamazepine, desipramine, duloxetine, escitalopram, imipramine, lamotrigine, memantine, moclobemide, quetiapine, reboxetine, risperidone, tianeptine, topiramate, trazodone |
| Adjunctive therapy* | Second-line: eszopiclone, olanzapine, risperidone Third-line: aripiprazole, clonidine, gabapentin, levetiracetam, pregabalin, quetiapine, reboxetine, tiagabine Not recommended: bupropion SR, guanfacine, topiramate, zolpidem |
| Not recommended | Alprazolam, citalopram, clonazepam, desipramine, divalproex, olanzapine (as monotherapy), tiagabine |
Guidelines
Acute and Post-Traumatic Stress Disorder Guidelines
| Guideline | Location | Year | Website | |
|---|---|---|---|---|
| Canadian Clinical Practice Guidelines | Canada | 2014 | - | Link |
| National Institute for Health and Care Excellence (NICE) | UK | 2018 | - | Link |
| American Psychiatric Association (APA) | USA | 2004, 2009 | - | • Guideline (2004) • Guideline Watch (2009) • Quick Reference |
| Veterans Affairs (VA) and Department of Defense (DoD) | USA | 2017 | - | Link |