- Last edited on May 18, 2020
Introduction to Antidepressants
Primer
Antidepressants are a class of medications used primarily in the treatment of mood disorders (e.g. - major depressive disorder) and anxiety disorders. Its use has expanded to neurodegenerative and neuropsychiatric disorders in recent years.
History
The development and history of antidepressants began in the 1950s, with the clinical use of two antidepressant drugs: iproniazid (a monoamine-oxidase inhibitor) and imipramine (a tricyclic antidepressant).[1] Iproniazid was used to treat tuberculosis at the time, but it was noticed that it also significantly improved the mood of patients, beyond just treating the medical illness. Imipramine, on the other hand, was discovered through a series of trials and errors by experimentation by Swiss psychiatrist Roland Kuhn.[2][3] These two discoveries heralded the first step towards psychopharmacology, as the only other major treatment that was available at the time was electroconvulsive therapy. The efficacy of these medications led to various theories on why the medications worked, including the monoamine hypothesis. TCAs and MAOis remained the mainstay of antidepressant treatment until the introduction of fluoxetine, a selective serotonin reuptake inhibitor, in the late 1980s.[4]
The SSRI Revolution
The introduction of the SSRIs revolutionized the treatment of depression and other psychiatric disorders, as these medications had a wider therapeutic index, and were more well tolerated with less side effects. However, there has been criticism (and rightly so) that this has led to an explosion of overdiagnosis and overtreatment,[5] especially in primary care settings, where there is very limited time for a detailed psychiatric history.[6][7]
Mechanism of Action
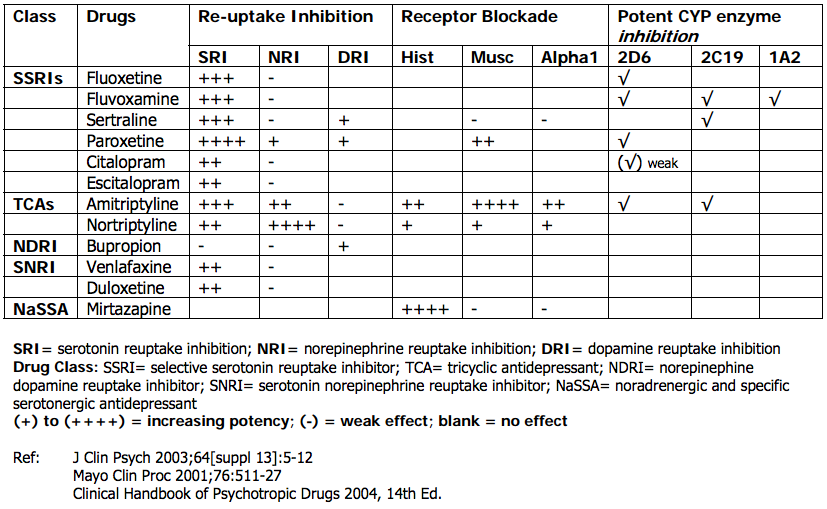
Given the wide range of classes of antidepressants, each of them have their own specific mechanism of action (see the individual drug pages for specifics). The key mechanism of action of most modern antidepressants is some modulation of serotonin reuptake, while others have more dopaminergic/noradrenergic effects (e.g - bupropion). Older antidepressants such as TCAs and MAOis also work by other mechanisms. For example, MAOis work by inhibiting monoamine oxidase, which slows the breakdown of norepinephrine, serotonin and dopamine in the brain.
Monoamine Hypothesis of Depression
Despite many decades of research, there is no single proven theory that supports the monoamine hypothesis. The monoamine hypothesis is too reductionistic and simplistic to explain complex a phenomenon like depression. Although the specific mechanism of how antidepressants improve mood, ahedonia, and neurovegetative symptoms is not well understood, the use of these medications remains indicated for treatment of psychiatric disorders, and are effective. Drawing parallels from other areas of medicine, general anesthesia has been used for over 160 years, yet there is still no formal understanding of the exact mechanism of how it works and why patients fall asleep.[8][9] There are also rare, but significant risks with use, such as memory impairment and death.[10] Despite this, general anesthesia remains in widespread use because of its benefits.
Antidepressant Classes
There are a many different classes of antidepressants. The landmark antidepressant trial, STAR*D, has shown that no one class of antidepressant is more effective than another.[11] The data from the this landmark is not without its criticisms, but it is the largest scale study of psychiatric medications that is available in the literature.[12] In general, most clinicians will pick a medication based on the patient's reported symptoms, comorbid diagnoses, tolerability to medications, previous response, drug–drug interactions, and the patient's own preference.[13] The cost of the medication should also be considered for patients with a lower socioeconomic background. Prescribing an antidepressant requires a detailed knowledge of pharmacology as well as drug-drug interactions. Other classes of antidepressants can be tailored according patient symptom profiles, such as using mirtazapine (which is sedating and an appetite stimulant) for patients who report poor appetite and sleep. Conversely, patients who have anxiety or anxious symptoms should avoid noradrenergic antidepressants (e.g. NDRIs such as bupropion). Paroxetine is generally not recommended as a first-line medication as it is very potent, and has the most severe withdrawal symptoms if the patient discontinues it abruptly.
SSRIs, SNRIs, NDRIs, MAOis, TCAs... What Do I Use?!
In terms of safety profile and prescribing practices, most clinicians now prescribe SSRIs, SNRIs, and other newer agents. Newer antidepressants generally have a better tolerability and safety profile. However, several decades ago, TCAs and MAOis were the predominant antidepressants. These medications remain effective for the treatment of depression, but are no longer in widespread use due to the narrow therapeutic index for TCAs, and the diet-restriction that is required with MAOi use (to prevent hypertensive crises). Experienced clinicians will be familiar using all classes of antidepressants and tailoring it to specific patient needs. The best antidepressant is the one that the patient actually uses.| SSRIs |
|---|
| Citalopram (Celexa) |
| Escitalopram (Cipralex/Lexapro) |
| Fluoxetine (Prozac) |
| Fluvoxamine (Luvox) |
| Paroxetine (Paxil) |
| Sertraline (Zoloft) |
| SNRIs |
|---|
| Duloxetine (Cymbalta) |
| Levomilnacipran (Fetzima) |
| Desvenlafaxine (Pristiq) |
| Venlafaxine (Effexor) |
| NDRIs |
|---|
| Bupropion (Wellbutrin) |
| NaSSAs |
|---|
| Mirtazapine (Remeron) |
Common Antidepressant Choices
| Escitalopram | Low side effect profile, good for treatment with comorbid medical illness.[14] Commonly prescribed in primary care settings. Unfortunately it has a narrow dose range (maximum 20mg), due to increased risk of QTc prolongation at higher doses. This means you can only increase the dose so much before needing to switch to another antidepressant if there is no response. |
|---|---|
| Sertraline | Good for patients with comorbid psychiatric diagnoses. Indicated as a first-line medication for not just depression, but also generalized anxiety, obsessive compulsive disorder, posttraumatic stress disorder, social anxiety disorder and other disorder. Sometimes felt by clinicians to be more sedating than other SSRIs, but the research evidence does not necessarily demonstrate this.[15] Sertraline has a higher incidence of GI side effects which can be mitigated by taking it with food, and with HS dosing, but this can be a reason for discontinuation. |
| Fluoxetine | Another good first-line choice and very similar to sertraline, with less GI side effects. It has the added benefit of also treating any comorbid eating disorders. It also has a long half-life, which means very little chance of withdrawal symptoms even if it is discontinued abruptly. |
Neurotransmitters and Neuroreceptors
From a neurotransmitter and physiology point of view, antidepressants with serotonin activity may help more with cognitive symptoms such as rumination, where as norephinephrine reuptake affects more of the behaviourial symptoms (anhedonia, low mood). TCAs have alpha blockade, which lead to postural hypotension, and dizziness. Mirtazapine has high histamine blockade which leads to drowsiness, weight gain, which sometimes can be used for the benefit of a patient's poor appetite and sleep.
Treatment
Length of Treatment
In the treatment of mood and anxiety disorders, some may experience benefits in the first six weeks of a treatment strategy, but full benefits may not be realized until 10 or 12 weeks have passed. During this time, doctors should work with their patients to adjust dosages so as to find an optimal level, and avoid stopping treatment prematurely. For a first episode of depression, the general recommended treatment timeline is 1 year. For a second episode, 2 years of treatment is recommended. For any third and subsequent episodes, lifetime treatment is recommended, as the risk of relapse is close to 100% off treatment.[16]
Monitoring
Patients should be carefully monitored every 1–2 weeks when first starting medications, as this is the period of greatest risk, including side effects. Treatment should be monitored with the routine use of validated outcome scales.
When Not to Treat
Switching/Tapering
Discontinuation
When a patient stops an antidepressant abruptly, antidepressant withdrawal (discontinuation syndrome) is a very clinically important phenomenon to monitor for. Different antidepressants will have different discontinuation side effects.[17] Psychiatric symptoms of discontinuation such as anxiety and agitation, crying spells, or irritability are also sometimes misdiagnosed as a depressive relapse. Antidepressants should thus be tapered slowly and on a schedule.
Side Effects and Adverse Events
Common
Excessive sweating can be common in patients on SSRIs and SNRIs.[18] In the elderly, falls can also be common with the use of SNRIs, TCAs, but less commonly in SSRIs.[19]
Education
It is important to educated patients about how medications work, and how side effects occur. It is important to remind patients that side effects start early in treatment, and the benefits of the medications come later (“Think of this as an investment in the future!”). There is huge variability in the side effect profiles that patients experience, despite our understandings of the psychopharmacology of these medications. What might work for one patient may not work for another.
Hyponatremia
The incidence of hyponatremia caused by SSRIs varies widely, from 0.5% to 32%. In the majority of cases, hyponatremia occurs within the first few weeks of the onset of therapy. The hyponatremia typically resolves 2 weeks after discontinuation of the SSRI.[20]
Sleep
- SSRIs can have idiosyncratic effects: can cause insomnia or agitation in any individual patient
- Up to 60% of patients on SSRIs are also on a hypnotic
- All SSRIs (plus SNRIs and TCAs, e.g. - amitriptyline, phenelzine, sertraline, venlafaxine) decrease sleep efficiency, increase REM latency, suppress REM, delay REM onset, increase number of awakenings, worsen PLMS and RLS, worsen parasomnias, and increase Stage 1 sleep
- Fluvoxamine and paroxetine are more sedating
- Fluoxetine is more stimulating
- Sertraline, citalopram and escitalopram are neutral
- SSRIs tend to increase extra-ocular movements (“Prozac eyes”)
Controversy
Placebo Effect?
In recent years, a popular and controversial theory has emerged through the media and the literature suggesting that modern antidepressants (SSRIs and beyond), do not exert any actual antidepressant effect (but is instead all driven by a placebo response and poor clinical studies).[21][22] Decades of research into the effects and mechanisms of antidepressants suggests that there are significant physiological mechanisms at work.[23] Prior to the development of SSRIs, tricyclic antidepressants and monoamine oxidase inhibitors were the dominant classes of antidepressants, and the efficacy of these medications were very well documented at the time.[24] The decades of research, latest large scale meta-analyses, and clinical evidence strongly disproves the theory that antidepressants are just a pure placebo.[25][26][27] The largest known study on antidepressant efficacy to date continues to support the efficacy and use for the acute treatment of adults with major depressive disorder.[28] More recent re-evaluation of placebo studies have shown that the placebo response rate has in fact has not increased over time.[29]
Despite the proven efficacy in short-term use, it is important to recognize there is a definite and strong placebo response to antidepressants. Most studies show a placebo response of anywhere from 30-40% in major depressive disorder.[30][31] However, it should also be noted this phenomenon is not just limited to psychiatry. The placebo effect is pervasive and apparently increasing throughout all areas of medicine. This includes sham surgeries in benign prostatic hyperplasia,[32] sham percutaneous coronary intervention in stable angina,[33] arthroscopy for osteoarthritis,[34] antiepileptic treatment of migraines,[35] bronchodilators for asthma,[36] and many others.[37][38] Just like with antidepressants, it does not mean that these treatments do not work, but that medicine is both an art and a science, and that every treatment decision requires clinical judgement and judicious use. The placebo response is poorly understood, and likely involves a complex interaction between neurobiologic mechanisms and the therapeutic doctor-patient interaction.[39]
Aggression and Suicidality
The role of antidepressants, specifically SSRIs, in causing aggression/violence and suicidality has long been debated since their introduction in the 1980s, especially in the popular media. [40] Studying aggression and suicidality is complicated, as human behaviour is complex and multifactorial. There are multiple confounding factors and variables that research cannot necessarily capture. A controversial paper was published in 2016 by Bielefeldt et al suggested that SSRIs doubled the risk of suicide/violence.[41] However, the paper was a meta-analysis that reviewed original papers. Importantly, there were no actual reported violent events or suicides, but adverse events (such as increased anxiety) were extrapolated to include the possibility that it could lead to violence/suicides.[42] Some have also hypothesized the role of akathisia in violence/agitation.[43][44] Other studies have shown a reduction in suicide ideation and behaviour with patients on SSRIs.[45]
A comprehensive review of the literature so far reveals scant evidence to support the hypothesis that modern antidepressants increase suicidality or aggression in adults.[46] However, evidence is clear that use in the pediatric population can result in increased agitation and suicidality. Therefore, antidepressants should never be used as a first-line treatment in children for mild-moderate depression, and psychosocial interventions should always be used first. There are valid concerns about prescribing antidepressants to children. In Canada, antidepressants have not been approved for individuals less than 18. In the United States, fluoxetine is the only antidepressant approved by the FDA for preadolescents (8 years and older). Escitalopram is also approved for children 12 years and older.
Paxil: A story of pharmaceutical influence
Despite the overall general safety of antidepressants, one antidepressant in particular has been in the spotlight in recent years and not for good reasons. Study 329,[47] a re-analysis in 2015 of the efficacy and safety of Paxil for children and adolescents showed that paroxetine (Paxil) was neither safe nor efficacious. In fact, there was significant harm exposed to the children, including increased suicidal ideation and behaviour. This important case is a reminder to clinicians of the huge role that pharmaceutical influence still has on healthcare (especially in the United States). Now more than ever, it is important to hold the industry accountable to drug studies so incidents like this are not repeated again. See also: Study 329 Working Group and Restoring Invisible and Abandoned Trials (RIAT)Research Supporting Antidepressants in Reducing Suicide Risk
Fetal Effects
Recent controversy has come up regarding concerns about the incidence of mental illness (autism, mood disorders, somatoform disorders, and behavioral disorders) in offspring of mothers taking SSRIs. Although animal studies of the neurobehavioral outcomes of fetal antidepressant exposure suggest mechanisms for such effects, most human studies indicate that maternal psychiatric illness account for much (but not all) of this risk. The fraction of cases attributable to antidepressant use (0.5%) is substantially lower than what would be attributable to parental psychiatric illness. Current treatment guidelines advise that antidepressants be used for severely ill mothers and advocate for discontinuation only in those with minimal illness/symptoms.[49][50]
Mortality
Ongoing research and clinicians have brought on concerns about antidepressants being generally harmful, because they disrupt ancient neurotransmitters such as serotonin, which plays a role in not just neurotransmission, but also other important bodily functions.[51] There are concerns that alterations to these ancient processes could potentially increase mortality.
Therefore, questions have been raised not necessarily about their short-term use, but the long-term health effects.[52] It is also important to recognize that antidepressants also have anticlotting properties that can be efficacious in treating cardiovascular disease and stroke. Various studies have in fact reinforced the importance of early treatment with antidepressants in post-stroke as it improves recovery.[53]